吉林大学学报(医学版) ›› 2025, Vol. 51 ›› Issue (5): 1303-1311.doi: 10.13481/j.1671-587X.20250517
• 临床研究 • 上一篇
静脉自控镇痛与布比卡因脂质体切口局部浸润麻醉对老年腰椎手术患者术后镇痛效果比较
- 1.吉林大学第一医院麻醉科,吉林 长春 130021
2.吉林大学第一医院脊柱外科,吉林 长春 130021
Comparison of postoperative analgesic efficacy between patient-controlled intravenous analgesia and liposomal bupivacaine incisional local infiltration anesthesia in elderly patients undergoing lumbar surgery
Liangbo WU1,Jieqiang ZHANG1,Changfeng FU2,Hushan WANG1( )
)
- 1.Department of Anesthesiology,First Hospital,Jilin University,Changchun 130021,China
2.Department of Spine Surgery,First Hospital,Jilin University,Changchun 130021,China
摘要:
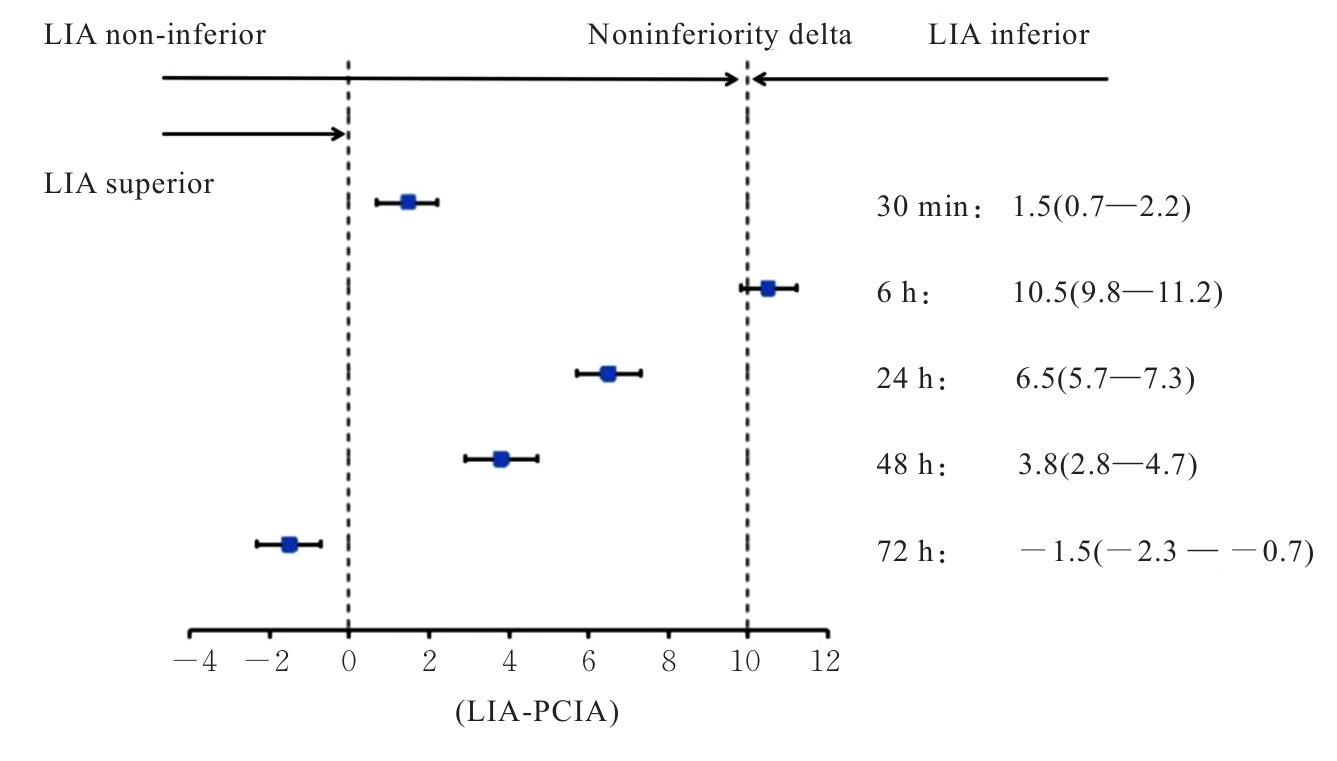
目的 比较接受单或双节段腰椎后路手术的老年患者分别应用舒芬太尼静脉自控镇痛(PCIA)与布比卡因脂质体切口局部浸润麻醉(LIA)的镇痛效果,为老年腰椎手术患者术后镇痛方法的选择提供依据。 方法 选取本院全麻下择期行单或双节段腰椎后路手术的老年患者124例,按照1∶1的比例将患者分为舒芬太尼PCIA组(PCIA组)和布比卡因脂质体切口LIA组(LIA组),每组各62例,除中途退出试验者外,最终PCIA组纳入58例患者,LIA组纳入60例患者。在手术结束前30 min,给予PCIA组患者舒芬太尼1.5 μg·kg-1联合右美托咪定1.5 μg·kg-1的镇痛泵方案治疗。术毕,LIA组患者由脊柱外科医生沿手术切口双侧多位点注射布比卡因脂质体266 mg(生理盐水40 mL稀释)。记录2组患者术后30 min、6 h、24 h、48 h和72 h的静息视觉模拟量表(VAS)疼痛评分(非劣效界值δ=10 mm)、术后不良反应(恶心呕吐、呼吸抑制、瘙痒、便秘和头晕嗜睡等)发生情况、术后补救镇痛次数、术后48和72 h麻醉满意度评分、术后住院时长及出院时切口愈合情况等。 结果 术后30 min~48 h,LIA组患者静息VAS疼痛评分均高于PCIA组(P<0.001),而LIA组患者术后72 h静息VAS疼痛评分低于PCIA组(P<0.001);术后30 min、24 h和48 h,非劣效性成立,布比卡因脂质体切口LIA的镇痛效果不劣于舒芬太尼PCIA;术后6 h,非劣效性不成立;术后72 h,布比卡因脂质体切口LIA的镇痛效果优于舒芬太尼PCIA(P<0.001);与PCIA组比较,LIA组患者术后恶心呕吐发生率降低(P<0.05),2组患者术后头晕嗜睡、便秘、呼吸抑制和瘙痒发生率比较差异无统计学意义(P>0.05);与PCIA组比较,LIA组患者术后住院时长缩短(P<0.001),2组患者术后补救镇痛次数和切口愈合等级比较差异无统计学意义(P>0.05);LIA组患者术后48和72 h麻醉满意度评分均高于PCIA组(P<0.05)。 结论 接受单或双节段腰椎手术的老年患者术后使用布比卡因脂质体切口LIA的镇痛效果并不劣于舒芬太尼PCIA,且术后不良反应发生率更低,术后镇痛满意度评分更高。
中图分类号:
- R614