| [1] |
MEGYESFALVI Z, GAY C M, POPPER H, et al. Clinical insights into small cell lung cancer: Tumor heterogeneity, diagnosis, therapy, and future directions[J]. CA Cancer J Clin, 2023, 73(6): 620-652.
|
| [2] |
MAISONNEUVE P, AGODOA L, GELLERT R, et al. Cancer in patients on dialysis for end-stage renal disease: an international collaborative study[J]. Lancet, 1999, 354(9173): 93-99.
|
| [3] |
TU H K, WEN C P, TSAI S P, et al. Cancer risk associated with chronic diseases and disease markers: prospective cohort study[J]. BMJ, 2018, 360: k134.
|
| [4] |
甘良英, 左 力. 血液透析人群中消除丙型肝炎病毒感染[J]. 临床肝胆病杂志, 2024, 40(4): 659-664.
|
| [5] |
DON Y, PYO L, MI L, et al. Cancer in Korean patients with end-stage renal disease: a 7-year follow-up[J]. PLoS One, 2017, 12(7): e0178649.
|
| [6] |
刘慧洁. 维持血液透析患者肿瘤发生及其相关因素的探讨[J]. 中华肿瘤防治杂志, 2018, 25(S2): 85, 87.
|
| [7] |
WANG L M, XU X, ZHANG M, et al. Prevalence of chronic kidney disease in China: results from the sixth China chronic disease and risk factor surveillance[J]. JAMA Intern Med, 2023, 183(4): 298-310.
|
| [8] |
THAI A A, SOLOMON B J, SEQUIST L V, et al. Lung cancer[J]. Lancet, 2021, 398(10299): 535-554.
|
| [9] |
MEIJER J J, LEONETTI A, AIRÒ G, et al. Small cell lung cancer: Novel treatments beyond immunotherapy[J]. Semin Cancer Biol, 2022, 86(Pt 2): 376-385.
|
| [10] |
LEE J H, SAXENA A, GIACCONE G. Advancements in small cell lung cancer[J]. Semin Cancer Biol, 2023, 93: 123-128.
|
| [11] |
TAKADA M, FUKUOKA M, KAWAHARA M, et al. Phase Ⅲ study of concurrent versus sequential thoracic radiotherapy in combination with cisplatin and etoposide for limited-stage small-cell lung cancer: results of the Japan Clinical Oncology Group Study 9104[J]. J Clin Oncol, 2002, 20(14): 3054-3060.
|
| [12] |
李雪芹, 张 凡, 李 倩. 免疫检查点抑制剂同步化疗治疗非小细胞肺癌效果及对患者肿瘤标志物和免疫细胞水平的影响[J]. 肿瘤研究与临床, 2023, 35(2): 99-103.
|
| [13] |
LAHIRI A, MAJI A, POTDAR P D, et al. Lung cancer immunotherapy: progress, pitfalls, and promises[J]. Mol Cancer, 2023, 22(1): 40.
|
| [14] |
PETTY W J, PAZ-ARES L. Emerging strategies for the treatment of small cell lung cancer: a review[J]. JAMA Oncol, 2023, 9(3): 419-429.
|
| [15] |
闫 焱, 焦碧航, 周 昆, 等. 基线BMI与免疫检查点抑制剂治疗晚期非小细胞肺癌疗效的关系[J]. 郑州大学学报(医学版), 2023, 58(3): 373-377.
|
| [16] |
ZHANG C Y, XU C, GAO X Y, et al. Platinum-based drugs for cancer therapy and anti-tumor strategies[J]. Theranostics, 2022, 12(5): 2115-2132.
|
| [17] |
VOLAREVIC V, DJOKOVIC B, JANKOVIC M G, et al. Molecular mechanisms of cisplatin-induced nephrotoxicity: a balance on the knife edge between renoprotection and tumor toxicity[J]. J Biomed Sci, 2019, 26(1): 25.
|
| [18] |
ZRAIK I M, HEß-BUSCH Y. Management of chemotherapy side effects and their long-term sequelae[J]. Urologe A, 2021, 60(7): 862-871.
|
| [19] |
CALVERT A H, NEWELL D R, GUMBRELL L A, et al. Carboplatin dosage: prospective evaluation of a simple formula based on renal function[J]. J Clin Oncol, 2023, 41(28): 4453-4454.
|
| [20] |
JANUS N, THARIAT J, BOULANGER H, et al. Proposal for dosage adjustment and timing of chemotherapy in hemodialyzed patients[J]. Ann Oncol, 2010, 21(7): 1395-1403.
|
| [21] |
LE T T, WU M L, LEE J H, et al. Etoposide promotes DNA loop trapping and barrier formation by topoisomerase Ⅱ[J]. Nat Chem Biol, 2023, 19(5): 641-650.
|
| [22] |
LIU S V, RECK M, MANSFIELD A S, et al. Updated overall survival and PD-L1 subgroup analysis of patients with extensive-stage small-cell lung cancer treated with atezolizumab, carboplatin, and etoposide (IMpower133)[J]. J Clin Oncol, 2021, 39(6): 619-630.
|
| [23] |
DOSTÁL Z, BUCHTÍKOVÁ J, MANDRLA J, et al. On the mechanism of miR-29b enhancement of etoposide toxicity in vitro [J]. Sci Rep, 2024, 14(1): 19880.
|
| [24] |
WANG J, ZHOU C C, YAO W X, et al. Adebrelimab or placebo plus carboplatin and etoposide as first-line treatment for extensive-stage small-cell lung cancer (CAPSTONE-1): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial[J]. Lancet Oncol, 2022, 23(6): 739-747.
|
| [25] |
CHENG Y, SPIGEL D R, CHO B C, et al. Durvalumab after chemoradiotherapy in limited-stage small-cell lung cancer[J]. N Engl J Med, 2024, 391(14): 1313-1327.
|
| [26] |
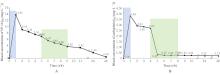
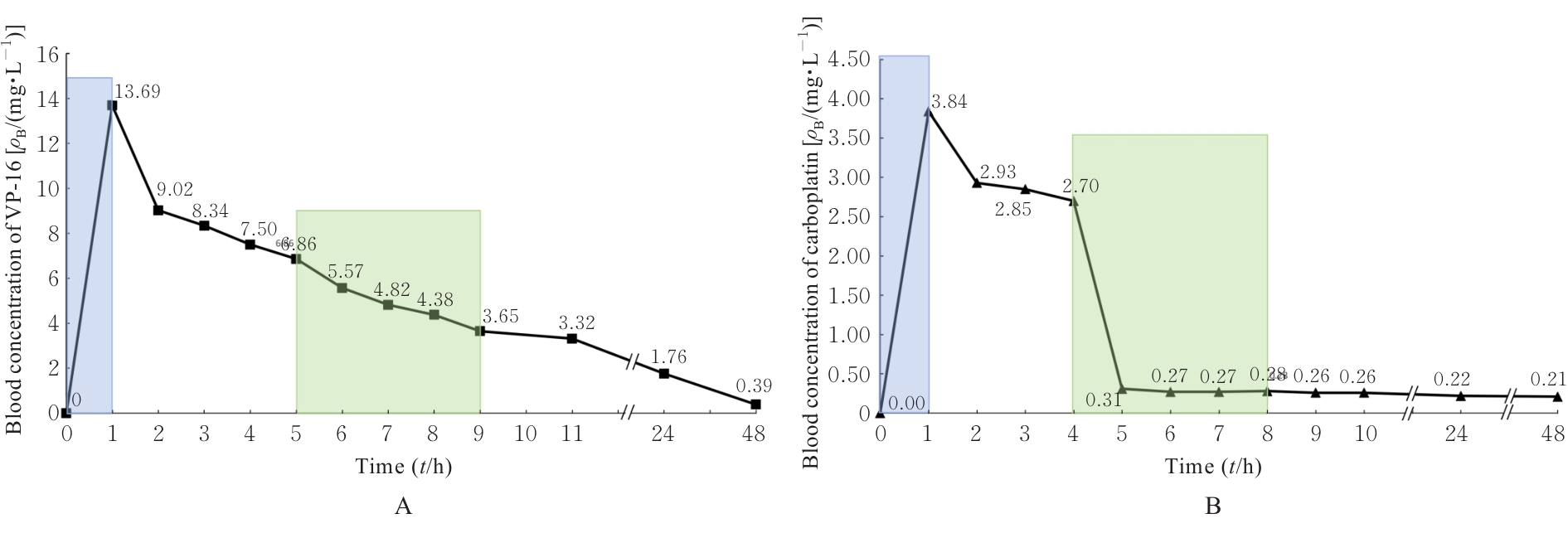
高 和, 纪树国, 王 峰, 等. 大剂量卡铂化疗的药代动力学[J]. 天津医药, 1998, 26(1): 32-34.
|
| [27] |
陆基宗, 许英华, 贺 晴, 等. 高效液相色谱法测定白血病人依托泊苷血药浓度及其药物动力学研究[J]. 中国现代应用药学, 2001, 18(1): 37-39.
|
| [28] |
QIN Z Y, REN G H, YUAN J J, et al. Systemic evaluation on the pharmacokinetics of platinum-based anticancer drugs from animal to cell level: based on total platinum and intact drugs[J]. Front Pharmacol, 2020, 10: 1485.
|
 ),Fengchun ZHANG1,2(
),Fengchun ZHANG1,2( )
)