| 1 |
CHALMERS S J, WYLAM M E. Methicillin-resistant Staphylococcus aureus infection and treatment options[J]. Methods Mol Biol, 2020,2069:229-251.
|
| 2 |
CANTY E, CARNAHAN B, CURLEY T, et al. Reduced vancomycin susceptibility, MRSA and treatment failure in pediatric staphylococcus aureus bloodstream infections[J]. Pediatr Infect Dis J, 2021, 40(5): 429-433.
|
| 3 |
RANJBAR R, ALAM M. Antimicrobial Resistance Collaborators (2022). Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis[J]. Evid Based Nurs, 2023: ebnurs-eb2022-103540.
|
| 4 |
胡付品,郭燕,朱德妹,等. 2021年CHINET中国细菌耐药监测[J]. 中国感染与化疗杂志, 2022,22(5):521-530.
|
| 5 |
申恩华,王立红,王辉,等.中国15个地区分离的耐甲氧西林金黄色葡萄球菌基因分型研究[J].中华流行病学杂志,2010(3):308-311.
|
| 6 |
陈泰尧,葛忆琳,刘雪薇,等.2017—2018年上海某医院耐甲氧西林金黄色葡萄球菌分子生物学特征研究[J].中华预防医学杂志,2020,54(8):849-853.
|
| 7 |
陈江华, 顾向明, 邓冲,等. 伤口与呼吸道医院感染金黄色葡萄球菌的耐药情况对比研究[J]. 中国抗生素杂志, 2012, 37(4):3.
|
| 8 |
BONAVENTURA G D, POMPILIO A, MONACO M,et al. Adhesion and biofilm formation by Staphylococcus aureus clinical isolates under conditions relevant to the host: relationship with macrolide resistance and clonal lineages[J]. J Med Microbiol, 2019, 68(2): 148-160.
|
| 9 |
POMORSKA-WESOŁOWSKA M, CHMIELARCZYK A, CHLEBOWICZ M, et al. Virulence and antimicrobial resistance of Staphylococcus aureus isolated from bloodstream infections and pneumonia in Southern Poland[J]. J Glob Antimicrob Resist, 2017, 11: 100-104.
|
| 10 |
李方去, 杨锦红, 王慧燕, 等. 两种临床标本中耐甲氧西林的金黄色葡萄球菌生物膜形成能力的检测与其耐药特征的研究[J]. 中国微生态学杂志, 2012, 24(6): 531-533.
|
| 11 |
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. M100-S32 [S]. Wayne,PA:CLSI,2022.
|
| 12 |
LAWAL O U, AYOBAMIY O, ABOUELFETOUH A,et al. A 6-year update on the diversity of methicillin-resistant Staphylococcus aureus clones in africa: A systematic review[J]. Front Microbiol,2022,3(13):860436.
|
| 13 |
RAO Q, SHANG W L, HU X M, et al. Staphylococcus aureus ST121: a globally disseminated hypervirulent clone[J]. J Med Microbiol, 2015,64(12): 1462-1473.
|
| 14 |
OGURA K, KAJI D, SASAKI M,et al.Predominance of ST8 and CC1/spa-t1784 methicillin-resistant staphylococcus aureus isolates in Japan and their genomic characteristics[J].J Glob Antimicrob Resist, 2022, 28:195-202.
|
| 15 |
KIM Y K, EOM Y, KIM E, et al. Molecular characteristics and prevalence of rifampin resistance in Staphylococcus aureus isolates from patients with bacteremia in South Korea[J]. Antibiotics (Basel),2023,12(10):1511.
|
| 16 |
CHONGTRAKOOL P, ITO T, MA X X, et al. Staphylococcal cassette chromosome mec (SCCmec) typing of methicillin-resistant Staphylococcus aureus strains isolated in 11 Asian countries: a proposal for a new nomenclature for SCCmec elements[J]. Antimicrob Agents Chemother, 2006, 50(3): 1001-1012.
|
| 17 |
IP M, YUNG R W, NG T K, et al. Contemporary methicillin-resistant Staphylococcus aureus clones in Hong Kong[J]. J Clin Microbiol, 2005, 43(10):5069-5073.
|
| 18 |
李文青, 程锦娥, 吴伟元, 等. 深圳地区甲氧西林耐药金黄色葡萄球菌耐药性及分子流行病学特征[J]. 中国人兽共患病学报, 2017, 33(12): 1098-1102.
|
| 19 |
DAI Y X, LIU J L, GUO W, et al. Decreasing methicillin-resistant Staphylococcus aureus (MRSA) infections is attributable to the disappearance of predominant MRSA ST239 clones, Shanghai, 2008-2017[J]. Emerg Microbes Infect, 2019, 8(1): 471-478.
|
| 20 |
LI X, ZHANG J, ZHANG Y, et al. Methicillin-resistant Staphylococcus aureus of the clonal lineage ST5-SCCmecⅡ-t2460 was associated with high mortality in a Wuhan hospital[J]. Braz J Microbiol,2021, 52(4):1929-1936.
|
| 21 |
WANG X, LI X, LIU W,et al. Molecular characteristic and virulence gene profiles of community-associated Methicillin-resistant Staphylococcus aureus isolates from pediatric patients in Shanghai, China[J]. Front Microbiol, 2016, 7: 1818.
|
| 22 |
LI X H, ZHANG J, ZHANG Y F, et al. Methicillin-resistant Staphylococcus aureus of the clonal lineage ST5-SCCmecⅡ-t2460 was associated with high mortality in a Wuhan hospital[J]. Braz J Microbiol, 2021, 52(4): 1929-1936.
|
| 23 |
ZHANG H, QIN L, JIN C, et al. Molecular Characteristics and antibiotic resistance of Staphylococcus aureus isolated from patient and food samples in Shijiazhuang, China[J]. Pathogens, 2022,11(11):1333.
|
| 24 |
OMUSE G, VAN ZYL K N, HOEK K,et al. Molecular characterization of Staphylococcus aureus isolates from various healthcare institutions in Nairobi, Kenya: a cross sectional study[J]. Ann Clin Microbiol Antimicrob, 2016, 15(1): 51.
|
| 25 |
陆军, 祝进, 徐礼锋,等. 社区与医院获得性耐甲氧西林金黄色葡萄球菌耐药性分析与比较[J]. 中国卫生检验杂志, 2012, 22(2):380-382.
|
| 26 |
CHEN Y, LIU Z X, DUO L B, et al. Characterization of Staphylococcus aureus from distinct geographic locations in China: an increasing prevalence of spa-t030 and SCCmec type Ⅲ[J]. PLoS One, 2014, 9(4): e96255.
|
| 27 |
LI Y M, ZHAO R K, ZHANG X F, et al. Prevalence of enterotoxin genes and spa genotypes of methicillin-resistant Staphylococcus aureus from a tertiary care hospital in China[J]. J Clin Diagn Res, 2015, 9(5): DC11-DC14.
|
| 28 |
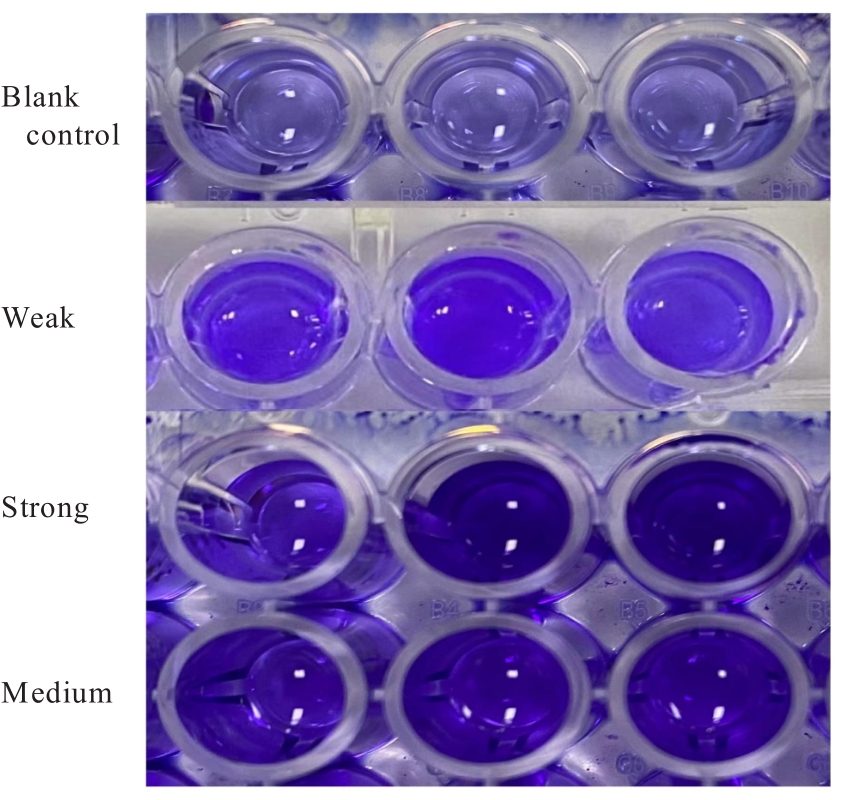
李文婷, 耿文静, 姚开虎, 等. 新生儿重症监护室金黄色葡萄球菌定植菌株的耐药性及生物膜形成能力研究[J]. 中国抗生素杂志, 2022, 47(3): 289-294.
|
| 29 |
ZHANG C, LI Z, PAN Q, et al. Berberine at sub-inhibitory concentration inhibits biofilm dispersal in Staphylococcus aureus [J]. Microbiology (Reading),2022,168(9). DOI: 10.1099/mic.0.001243 .
doi: 10.1099/mic.0.001243
|
| 30 |
BHATTACHARYA S, BIR R, MAJUMDAR T. Evaluation of multidrug resistant staphylococcus aureus and their association with biofilm production in a tertiary care hospital, Tripura, northeast India[J]. J Clin Diagn Res, 2015, 9(9): DC01-DC04.
|
 ),王俊瑞3(
),王俊瑞3( )
)
 ),Junrui WANG3(
),Junrui WANG3( )
)