| [1] |
Siqi LI,Guangdao CHEN,Qiyi ZENG.
Improvement effect of chrysophanol on hydrogen peroxide-induced apoptosis of EA. hy926 cells and its mechanism
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(6): 1512-1518.
|
| [2] |
Fangyang JIANG,Jing XIAO,He CHANG,Mingyang SUN,Wenjing ZHANG,Guangfu LYU,He LIN,Zhe LIN,Xiaowei HUANG,Yuchen WANG.
Effect of polygonatum odoratum polysaccharide on acute kidney injury in mice induced by cisplatin and its ferroptosis mechanism
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(5): 1235-1242.
|
| [3] |
Haoyu WANG,Yuqi WANG,Bingqian WANG,Jinhan NIE,Jiaqing YAN,Min HU.
Inhibitory effect of mesalazine on pro-inflammatory factors and peroxides in RAW264.7 cells and its therapeutic effect on periodontitis model rats
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(5): 1250-1258.
|
| [4] |
Fengmei XIONG,Yuxiang CAI,Zhuo LIU,Na SUN,Yang LI.
Alleviatory effect of curcumin on cardiomyocyte toxicity induced by doxorubicin by regulating SIRT3/SOD2 signaling pathway
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(5): 1339-1347.
|
| [5] |
Zhifei LIU,Yaru BI,Chenglin SUN,Suyan TIAN.
Mendelian randomization analysis based on causal relationship between gut microbiota and gestational diabetes mellitus
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(5): 1381-1389.
|
| [6] |
Xueting CHI,Fangyuan CHEN,Zifeng PI,Guangfu LYU,Yuchen WANG,Yinqing LI,Xiaowei HUANG,Zhe LIN.
Improvement effect of velvet antler polypeptide on postmenopausal osteoporosis in rats and its mechanism
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(4): 963-969.
|
| [7] |
Jianan HAN,Zhuorui LIU,Peiyong ZENG,Shuang JIANG,Hongyu LI.
Anti-fatigue effect of Wujia Shengmai Yin in mice and its mechanism
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(3): 689-696.
|
| [8] |
Jing TANG,Huan LI,Shuo ZHANG,Ligang JING.
Analysis on association between serum homocysteine and inflammatory response and oxidative stress in patients with acute ischemic stroke
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(3): 786-790.
|
| [9] |
Yingxin RUAN,Junya JIA,Zhanfei WU,Wenya SHANG,Pengyu ZHANG.
Effect of NLRP3 inflammatome in renal interstitial fibrosis induced by unilateral ureteral obstruction in rats and its mechanism
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(3): 587-595.
|
| [10] |
Yuexin LIU,Yongwei LAI,Yanchun WANG,Bo XU,Qian LU,Ying AN,Kuang REN,Hongyan FAN.
Improvement effect of total flavonoids of Sophora flavescens on oxidative stress induced by lead acetate in leydig cells in mice and its in effect on Keap1/Nrf2 signaling pathway
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(2): 320-325.
|
| [11] |
Xue FANG,Yu KANG,Xiaoxi SHA,Zhifen HAN,Yan ZHANG.
Detection of gastrocnemius muscle hardness of diabetic patients under different functional states by ultrasonic shear wave elastography and its clinical significance
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(2): 451-456.
|
| [12] |
Xueting CHI,Xiaowei HUANG,Fangyuan CHEN,Gaofeng ZHOU,Jinji WANG,Guangfu LYU,Zhe LIN,Qing GONG.
Improvement effect of velvet antler polypeptide in osteoporosis model rats and its effect on SIRT1/FOXO1 signaling pathway
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(1): 120-127.
|
| [13] |
Li LIU,Linsheng HUANG,Yongheng ZHAO,Wenjie CAO,Yongshuai QIAN,Huifan YU,Fei LI.
Network pharmacological analysis on Balanophora involucrataHook.f. in treatment of hyperuricemia and its therapeutic effect on hyperuricemia cell model and hyperuricemia model mouse
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(1): 58-70.
|
| [14] |
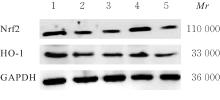
Weichen HOU,Guimei ZHANG,Shushi ZHANG.
Inhibitory effect of gingerone on apoptosis of HT22 cells by alleviation oxidative stress damage after OGD/R through activating Nrf2/HO-1 signaling pathway
[J]. Journal of Jilin University(Medicine Edition), 2024, 50(1): 97-105.
|
| [15] |
Wenting HUI,Tongtong SONG,Min HUANG,Xia CHEN.
Effect of hydrogel-based delivery of bFGF on function of NIH3T3 cells after oxygen-glucose deprivation
[J]. Journal of Jilin University(Medicine Edition), 2023, 49(6): 1484-1490.
|
 )
)