Journal of Jilin University(Medicine Edition) ›› 2025, Vol. 51 ›› Issue (3): 763-769.doi: 10.13481/j.1671-587X.20250321
• Research in clinical medicine • Previous Articles
Analysis on risk factors of development of acute hydrocephalus in patients with aneurysmal subarachnoid hemorrhage
Jiahui FENG,Renjie LIU,Xuan CHEN( )
)
- Department of Neurovascular Disease,First Hospital,Jilin University,Changchun 130021,China
-
Received:2024-06-17Accepted:2024-08-30Online:2025-05-28Published:2025-07-18 -
Contact:Xuan CHEN E-mail:chen_xuan@jlu.edu.cn
CLC Number:
- R651.1
Cite this article
Jiahui FENG,Renjie LIU,Xuan CHEN. Analysis on risk factors of development of acute hydrocephalus in patients with aneurysmal subarachnoid hemorrhage[J].Journal of Jilin University(Medicine Edition), 2025, 51(3): 763-769.
share this article
Tab.1
General informations of patients in aHCP group and non-aHCP group"
| Clinical data | aHCP group (n=56) | Non-aHCP group (n=119) | t /Z/χ2 | P | |
|---|---|---|---|---|---|
| Age(year) | 60.361±8.814 | 59.131±10.097 | -0.783 | ||
| Female(n/%) | 34(60.7) | 86(72.3) | 2.469 | ||
| Hypertension(n/%) | 31(55.4) | 57(47.5) | 0.943 | ||
| Location of aneurysm(n/%) | 4.465 | ||||
| ACoA | 12(21.4) | 41(34.5) | |||
| PCoA | 20(35.7) | 33(27.7) | |||
| ACA | 6(10.7) | 9(7.6) | |||
| MCA | 12(21.4) | 24(20.2) | |||
| Posterior circulation aneurysm | 6(10.7) | 12(10.1) | |||
| Intraventricular hemorrhage (n/%) | 33(58.9) | 43(36.1) | 8.301 | ||
| Hunt-Hess grade (n/%) | 25.701 | <0.001 | |||
| Ⅰ/Ⅱ | 37(66.1) | 96(80.7) | |||
| Ⅲ/Ⅳ | 19 (33.9) | 23(19.3) | |||
| Modified Fisher grade (n/%) | 26.682 | <0.001 | |||
| Ⅰ/Ⅱ | 36(64.3) | 93(78.2) | |||
| Ⅲ/Ⅳ | 20(35.7) | 26(21.8) | |||
| Laboratory testing | |||||
| RDW [n/%, M (P25, P75)] | 12.55(12.30,13.18) | 12.60(12.20,13.20) | -0.114 | 0.909 | |
| NE#(×109 L-1, x±s) | 12.63±3.56 | 8.60±2.96 | -7.864 | <0.001 | |
| LY#(×109 L-1, x±s) | 0.81(0.66,1.01) | 1.10(0.88,1.67) | -4.973 | <0.001 | |
| MO#(×109 L-1, x±s) | 0.51±0.29 | 0.47±0.23 | -1.075 | 0.284 | |
| FBG [g?L-1, x±s] | 2.91±0.73 | 2.81±0.69 | -0.872 | 0.385 | |
| Albumin [ρB/(g?L-1), x±s] | 42.79±3.52 | 42.35±3.21 | -0.817 | 0.471 | |
| Serum sodium [mmol?L-1, M (P25, P75)] | 137.00(135.90,139.50) | 137.75(136.33,140.03) | -1.223 | 0.221 | |
| Blood glucose [mmol?L-1, M (P25, P75)] | 7.52(6.29,9.20) | 6.66(5.79,8.18) | -2.5 | 0.012 | |
| NAR (x±s) | 0.295±0.081 | 0.202±0.068 | -7.956 | <0.001 | |
| PLR [M (P25, P75)] | 281.13(225.88,387.02) | 187.40(127.03,252.05) | -5.574 | <0.001 | |
| NLR [M (P25, P75)] | 15.73(11.57,20.17) | 7.80(4.07,11.96) | -7.330 | <0.001 | |
| MLR [M (P25, P75)] | 0.60(0.37,0.76) | 0.36(0.26,0.49) | -4.731 | <0.001 | |
| FAR [M (P25, P75)] | 0.067(0.057,0.078) | 0.061(0.054,0.076) | -0.704 | 0.482 | |
| SII [M (P25, P75)] | 3 557.22(2 449.00,5 016.03) | 1 656.14(864.80,2 458.38) | -7.272 | <0.001 | |
| SIRI [M (P25, P75)] | 6.66(3.88,10.25) | 2.87(1.76,4.80) | -6.229 | <0.001 | |
| AISI [M (P25, P75)] | 1 605.69(878.82,2 398.48) | 637.84(364.09,1 034.62) | -6.140 | <0.001 | |
Tab. 2
Independent variable and dependent variable assignments of binary Logistic regression analysis"
| Factor | Assignment method |
|---|---|
| Dependent variable | Non-aHCP group=0; aHCP group=1 |
| Independent variables | |
| Intraventricular hemorrhage | NO=0, YES=1 |
| Hunt-Hess grade | Ⅰ/Ⅱ=0, Ⅲ/Ⅳ=1 |
| Modified Fisher grade | Ⅰ/Ⅱ=0, Ⅲ/Ⅳ=1 |
NE# LY# | Continuous variable Continuous variable |
Blood glucose NAR PLR NLR MLR | Continuous variable Continuous variable Continuous variable Continuous variable Continuous variable |
SII SIRI AISI | Continuous variable Continuous variable Continuous variable |
Tab. 3
Binary Logistic regression analysis on influencing factors of aHCP in aSAH patients"
| Variable | b | SE | Wald χ2 | OR (95%CI) | P |
|---|---|---|---|---|---|
| Intraventricular hemorrhage | 0.384 | 0.481 | 0.638 | 1.468(0.572-3.765) | 0.425 |
| Hunt-Hess grade | 1.160 | 0.635 | 3.339 | 3.191(0.919-11.079) | 0.068 |
| Modified Fisher grade | 0.445 | 0.545 | 0.667 | 1.561(0.536-4.546) | 0.414 |
| NE# | 0.133 | 0.366 | 0.131 | 1.142(0.558-2.338) | 0.717 |
| LY# | 0.277 | 0.890 | 0.097 | 1.319(0.231-7.550) | 0.755 |
| Blood glucose | 0.076 | 0.106 | 0.529 | 1.079(0.875-1.332) | 0.477 |
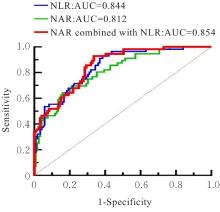
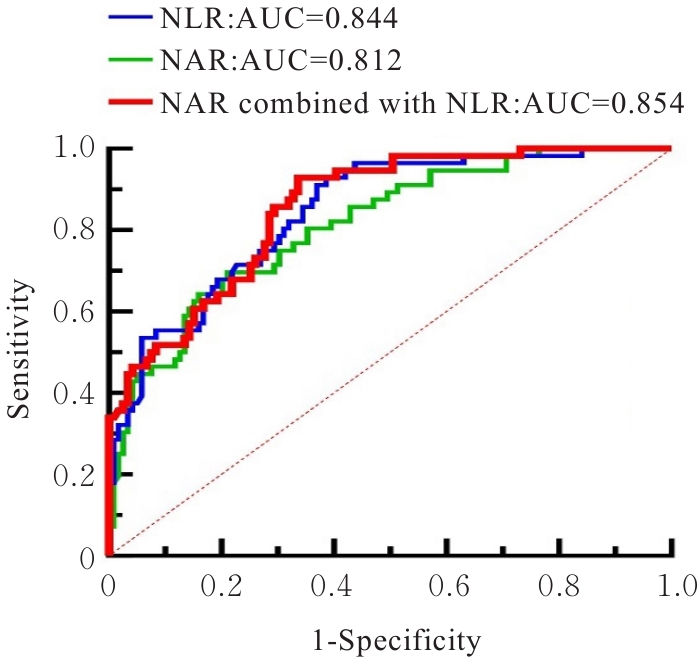
| NAR | 0.805 | 0.380 | 4.502 | 2.237(1.063-4.708) | 0.034 |
| PLR | 0.009 | 0.008 | 1.356 | 1.009 (0.997-1.031) | 0.244 |
| NLR | 0.190 | 0.051 | 13.931 | 1.210(1.095-1.337) | <0.001 |
| MLR | 1.175 | 0.835 | 2.050 | 3.238(0.630-16.638) | 0.159 |
| SII | 0.000 | 0.001 | 0.217 | 1.000(0.998-1.003) | 0.641 |
| SIRI | -0.236 | 0.502 | 0.220 | 0.790(0.295-2.114) | 0.790 |
| AISI | 0.001 | 0.002 | 0.097 | 1.001(0.997-1.005) | 0.725 |
| [1] | WANG J Y, ZHANG X T, WANG J Q, et al. Admission neutrophil-lymphocyte ratio predicts rebleeding following aneurismal subarachnoid hemorrhage[J]. World Neurosurg, 2020, 138: e317-e322. |
| [2] | CUOCO J A, GUILLIAMS E L, KLEIN B J, et al. Monocyte count on admission is predictive of shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage[J]. Front Surg, 2022, 9: 879050. |
| [3] | HOH B L, KO N U, AMIN-HANJANI S, et al. 2023 guideline for the management of patients with aneurysmal subarachnoid hemorrhage: a guideline from the American heart association/American stroke association[J]. Stroke, 2023, 54(7): e314-e370. |
| [4] | LOLANSEN S D, ROSTGAARD N, CAPION T, et al. Posthemorrhagic hydrocephalus in patients with subarachnoid hemorrhage occurs independently of CSF osmolality[J]. Int J Mol Sci, 2023, 24(14): 11476. |
| [5] | JOVANOVIĆ I, NEMIR J, GARDIJAN D, et al. Transient acute hydrocephalus after aneurysmal subarachnoid hemorrhage and aneurysm embolization: a single-center experience[J]. Neuroradiology, 2021, 63(12): 2111-2119. |
| [6] | CHOU S H, LOCH MACDONALD R, KELLER E, et al. Biospecimens and molecular and cellular biomarkers in aneurysmal subarachnoid hemorrhage studies: common data elements and standard reporting recommendations[J]. Neurocrit Care, 2019, 30(): 46-59. |
| [7] | WU Y, HE Q G, WEI Y L, et al. The association of neutrophil-to-lymphocyte ratio and delayed cerebral ischemia in patients with aneurysmal subarachnoid hemorrhage: possible involvement of cerebral blood perfusion[J]. Neuropsychiatr Dis Treat, 2019, 15: 1001-1007. |
| [8] | HOU F D, ZHANG Q Q, ZHANG W W, et al. A correlation and prediction study of the poor prognosis of high-grade aneurysmal subarachnoid hemorrhage from the neutrophil percentage to albumin ratio[J]. Clin Neurol Neurosurg, 2023, 230: 107788. |
| [9] | ZHANG Y B, ZHENG S F, WANG H J, et al. Admission lower serum phosphate ion levels predict acute hydrocephalus of aneurysmal subarachnoid hemorrhage[J]. Front Neurol, 2022, 12: 759963. |
| [10] | 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组, 中华医学会神经病学分会神经血管介入协作组. 中国蛛网膜下腔出血诊治指南2019 [J]. 中华神经科杂志, 2019, (12): 1006-1021. |
| [11] | HOCHSTETLER A, RASKIN J, BLAZER-YOST B L. Hydrocephalus: historical analysis and considerations for treatment[J]. Eur J Med Res, 2022, 27(1): 168. |
| [12] | PALASZ J, D’ANTONA L, FARRELL S, et al. External ventricular drain management in subarachnoid haemorrhage: a systematic review and meta-analysis[J]. Neurosurg Rev, 2022, 45(1): 365-373. |
| [13] | LUCKE-WOLD B P, LOGSDON A F, MANORANJAN B, et al. Aneurysmal subarachnoid hemorrhage and neuroinflammation: a comprehensive review[J]. Int J Mol Sci, 2016, 17(4): 497. |
| [14] | LI X, CHEN G. CNS-peripheral immune interactions in hemorrhagic stroke[J]. J Cereb Blood Flow Metab, 2023, 43(2): 185-197. |
| [15] | TAO C Y, WANG J J, HU X, et al. Clinical value of neutrophil to lymphocyte and platelet to lymphocyte ratio after aneurysmal subarachnoid hemorrhage[J]. Neurocrit Care, 2017, 26(3): 393-401. |
| [16] | CUOCO J A, GUILLIAMS E L, KLEIN B J, et al. Neutrophil count on admission predicts acute symptomatic hydrocephalus after aneurysmal subarachnoid hemorrhage[J]. World Neurosurg, 2021, 156: e338-e344. |
| [17] | SAAND A R, YU F, CHEN J, et al. Systemic inflammation in hemorrhagic strokes-A novel neurological sign and therapeutic target?[J]. J Cereb Blood Flow Metab, 2019, 39(6): 959-988. |
| [18] | JAMALI S A, TURNBULL M T, KANEKIYO T, et al. Elevated neutrophil-lymphocyte ratio is predictive of poor outcomes following aneurysmal subarachnoid hemorrhage[J]. J Stroke Cerebrovasc Dis, 2020, 29(4): 104631. |
| [19] | ZHANG X, ZHANG S, WANG C K, et al. High neutrophil-to-albumin ratio predicts postoperative pneumonia in aneurysmal subarachnoid hemorrhage[J]. Front Neurol, 2022, 13: 840858. |
| [20] | GUO Y H, LIU J, ZENG H H, et al. Neutrophil to lymphocyte ratio predicting poor outcome after aneurysmal subarachnoid hemorrhage: a retrospective study and updated meta-analysis[J]. Front Immunol, 2022, 13: 962760. |
| [21] | HOU Y Y, FAN J X, YUAN H S, et al. Prognostic capacity of the systemic inflammation response index for functional outcome in patients with aneurysmal subarachnoid hemorrhage[J]. Front Neurol, 2023, 14: 1054315. |
| [22] | LATTANZI S, CAGNETTI C, RINALDI C, et al. Neutrophil-to-lymphocyte ratio improves outcome prediction of acute intracerebral hemorrhage[J]. J Neurol Sci, 2018, 387: 98-102. |
| [23] | GUSDON A M, SAVARRAJ J P J, SHIHABEDDIN E, et al. Time course of peripheral leukocytosis and clinical outcomes after aneurysmal subarachnoid hemorrhage[J]. Front Neurol, 2021, 12: 694996. |
| [24] | ZHANG X, ZHANG S, WANG C K, et al. Neutrophil-to-albumin ratio as a novel marker predicting unfavorable outcome in aneurysmal subarachnoid hemorrhage[J]. J Clin Neurosci, 2022, 99: 282-288. |
| [25] | ZHANG R J, LIU Z R, ZHANG Y, et al. Improving the models for prognosis of aneurysmal subarachnoid hemorrhage with the neutrophil-to-albumin ratio[J]. Front Neurol, 2023, 14: 1078926. |
| [1] | Suzhen YUAN,Yan JIN,Wenwen WANG. Analysis on clinical characteristics of patients with ovarian clear cell carcinoma and ovarian endometriosis [J]. Journal of Jilin University(Medicine Edition), 2024, 50(6): 1677-1682. |
| [2] | Honghong LI,Na YU,Minghao SHI,Ying SUN,Yao LI,Zhongjun SHEN,Xiaoyi LIU,Liyan ZHAO. Predictive value of new thrombotic risk assessment model for venous thromboembolism in patients with malignant tumors [J]. Journal of Jilin University(Medicine Edition), 2024, 50(5): 1390-1399. |
| [3] | Jiayuan YU,Di ZHAO,Xin JIANG,Jing XU,Lili JIANG,Hongyu JIANG. Association analysis on peripheral blood lymphocyte subsets and occurrence of carotid atherosclerosis [J]. Journal of Jilin University(Medicine Edition), 2024, 50(5): 1400-1405. |
| [4] | Peng QI,Xianying MENG,Meihua PIAO,Qiang ZHANG. Network Meta-analysis on risk factors of recurrence of papillary thyroid microcarcinoma [J]. Journal of Jilin University(Medicine Edition), 2023, 49(6): 1504-1512. |
| [5] | Xiunan FENG,Lu CHEN,Yu LONG,Zhenyu JIANG,Ling ZHAO. Analysis on clinical characteristics and risk factors of patients with Sjogren’s syndrome complicated with interstitial lung disease [J]. Journal of Jilin University(Medicine Edition), 2023, 49(6): 1513-1518. |
| [6] | Xue DONG, Jinfeng ZANG, Caifeng XU, Hebing LIU, Zhaohua CHENG. Construction and validation of risk prediction model of enteral nutrition feeding intolerance of patients with severe acute pancreatitis [J]. Journal of Jilin University(Medicine Edition), 2023, 49(6): 1586-1592. |
| [7] | Tong SHEN,Yang WANG,Wei JIN,Zhihui LIN,Li YAN. Risk factors analysis and risk model construction of cognitive frailty in elderly patients with chronic diseases [J]. Journal of Jilin University(Medicine Edition), 2023, 49(5): 1304-1309. |
| [8] | Mingfei JU,Chao LIU,Zhigang MA,Juan ZHAO,Tu WANG,Zhihao WANG. Predictive value of residual cholesterol in occurrence of patients with acute coronary syndrome [J]. Journal of Jilin University(Medicine Edition), 2023, 49(3): 765-769. |
| [9] | Lianyuan WANG,Yi YANG,Huiwen CONG,Haohua WANG,Qihan BAO,Chengsheng LI,Liwen ZHOU,Zichen DING,Yanli LI,Fuyan SHI,Suzhen WANG. Bayesian quantile regression joint model analysis on risk factors of Alzheimer’s disease in people with different MMSE scores [J]. Journal of Jilin University(Medicine Edition), 2023, 49(2): 395-401. |
| [10] | Shan GAO,Yutong WANG,Minqiu LU,Lei SHI,Bin CHU,Yuehua DING,Mengzhen WANG,Li BAO. Analysis on causes for early death and its risk factors of patients with multiple myeloma in era of novel drugs [J]. Journal of Jilin University(Medicine Edition), 2022, 48(3): 783-789. |
| [11] | ZHANG Haolong, YU Zhentao, GAO Zihan, WU Yuanyu, FANG Xuedong. Related risk factors and clinical treatment of patients with PGS after gastric cancer operation [J]. Journal of Jilin University(Medicine Edition), 2019, 45(03): 673-677. |
| [12] | JIANG Rui, LIU Fang, PAN Yueji, LU Boyang, HOU Lulu, WANG Chunmei, JIA Hui, SHI Xiaoru. Screening and analysis of dry eye in eye discomfort patients in Jilin Province [J]. Journal of Jilin University Medicine Edition, 2017, 43(04): 832-838. |
| [13] | ZHOU Hong, LIU Jincai, LUO Guanghua, XIE Peihan, YANG Juan, DONG Yulan, QING Weipeng, ZHANG Jingjing. Application of Coronary Artery Disease-Reporting and Data System in risk factor analysis of patients with coronary artery disease [J]. Journal of Jilin University Medicine Edition, 2017, 43(03): 617-622. |
| [14] | SI Henan, ZHONG Shuxia, ZHOU Junfeng, YAO Lei, LIU Yuanyuan, SONG Yang, LI Shanshan. Analysis on clinical characteristics and risk factors of 271 children with vitiligo [J]. Journal of Jilin University Medicine Edition, 2017, 43(01): 147-150. |
| [15] | GUO Li, ZHANG Xiaoxia, YU Meiling, ZHAO Ting, ZHANG Liqun. Preventive effect of hydroxyethyl starch solution on ovarian hyperstimulation syndrome [J]. Journal of Jilin University Medicine Edition, 2016, 42(06): 1147-1150. |
|
||