| 1 |
SMITH TJ HL. Graves’ Disease[J]. N Engl J Med, 2016, 375(16):1552-1565.
|
| 2 |
CONSTANTINESCU S M, HOSPEL J, DAUMERIE C, et al. Significance of thyroperoxidase and thyroglobulin antibodies in medically treated Graves’ disease[J]. Eur Thyroid J, 2023, ETJ-23-0193.
|
| 3 |
HOANG T D, STOCKER D J, CHOU E L, et al. 2022 update on clinical management of Graves disease and thyroid eye disease[J]. Endocrinol Metab Clin North Am, 2022, 51(2): 287-304.
|
| 4 |
沈 维, 朱 远, 刘 昭, 等. 药物难治性Graves病 131I 治疗疗效分析[J]. 标记免疫分析与临床, 2023, 30(9): 1454-1460.
|
| 5 |
LI P, WANG W, YAN M Q, et al. Different doses of methimazole treatment of children and adolescents with Graves’ disease: a clinical study based on 161 cases of outpatients[J]. BMC Endocr Disord, 2023, 23(1): 233.
|
| 6 |
VICENTE N, CARDOSO L, BARROS L, et al. Antithyroid drug-induced agranulocytosis: state of the art on diagnosis and management[J]. Drugs R D, 2017, 17(1): 91-96.
|
| 7 |
CHAUDHRY L A, MAUZEN K F, BA-ESSA E, et al. Antithyroid drug induced a granulocytosis: what still we need to learn?[J]. Pan Afr Med J, 2016, 23: 27.
|
| 8 |
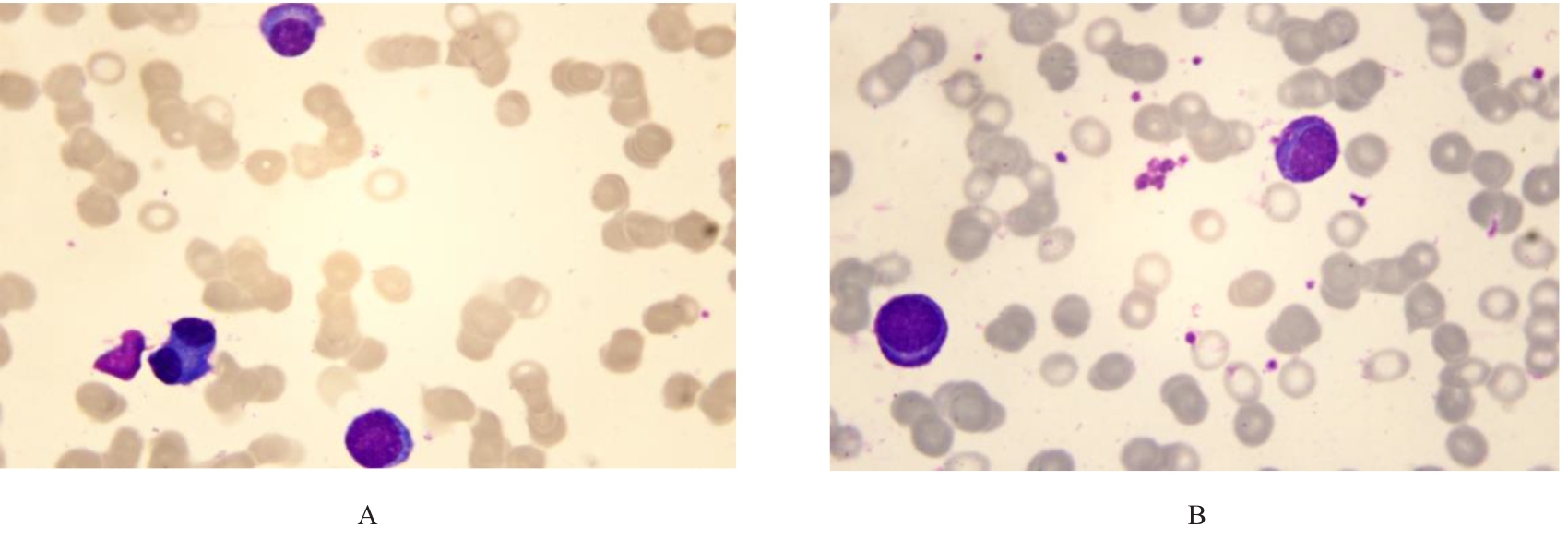
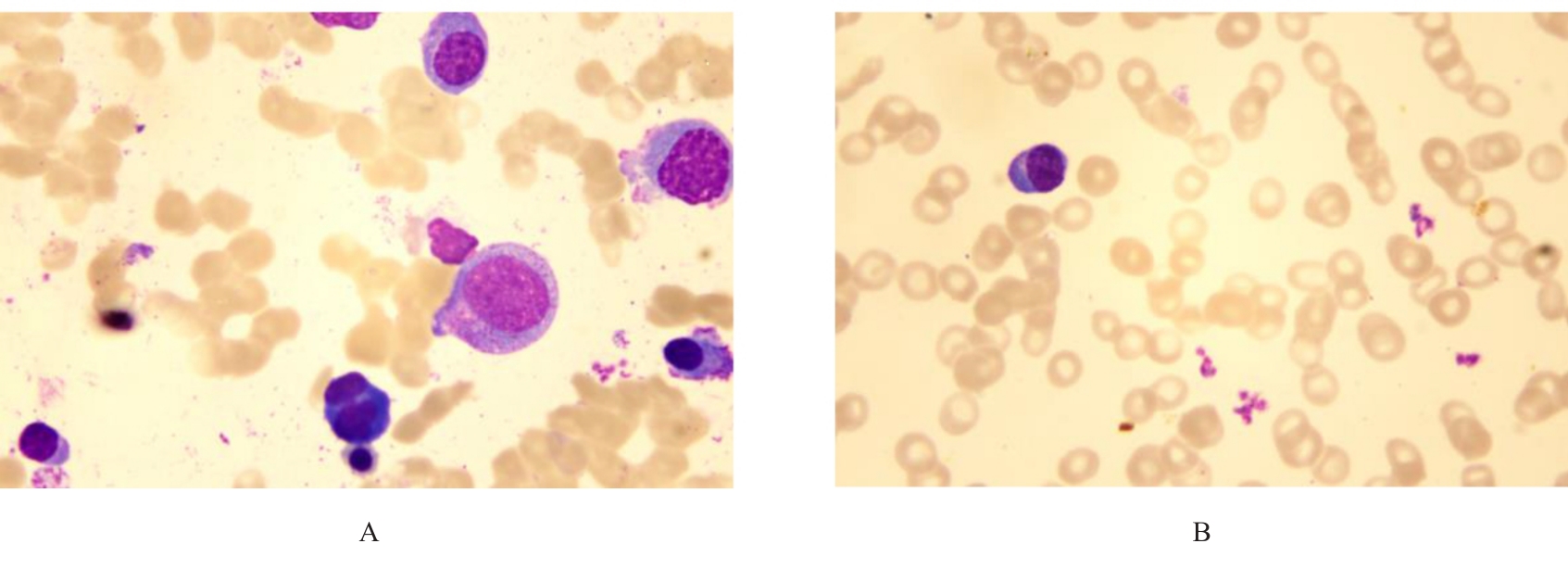
XIAO F, LI C Y, YOU L S, et al. Massive plasmacytosis with severe marrow suppression induced by methimazole in Graves’ disease patients: case report and literature review[J]. Int J Clin Exp Med, 2014, 7(10): 3605-3608.
|
| 9 |
BREIER D V, RENDO P, GONZALEZ J, et al. Massive plasmocytosis due to methimazole-induced bone marrow toxicity[J]. Am J Hematol, 2001, 67(4): 259-261.
|
| 10 |
YAMAMOTO A, KATAYAMA Y, TOMIYAMA K, et al. Methimazole-induced aplastic anemia caused by hypocellular bone marrow with plasmacytosis[J]. Thyroid, 2004, 14(3): 231-235.
|
| 11 |
OH E J, CHAE H J, PARK Y J, et al. Agranulocytosis, plasmacytosis, and thrombocytosis due to methimazole-induced bone marrow toxicity[J]. Am J Hematol, 2007, 82(6): 500.
|
| 12 |
KHINE A, DHILLON K, JO L, et al. Two cases of methimazole-induced agranulocytosis with their risk factors[J]. AACE Clin Case Rep, 2022, 8(2): 82-84.
|
| 13 |
YANG J, ZHU Y J, ZHONG J J, et al. Characteristics of antithyroid drug-induced agranulocytosis in patients with hyperthyroidism: a retrospective analysis of 114 cases in a single institution in China involving 9 690 patients referred for radioiodine treatment over 15 years[J]. Thyroid, 2016, 26(5): 627-633.
|
| 14 |
GARCÍA GÓMEZ C, NAVARRO E, ALCÁZAR V, et al. Therapeutic management and long-term outcome of hyperthyroidism in patients with antithyroid-induced agranulocytosis: a retrospective, multicenter study[J]. J Clin Med, 2023, 12(20): 6556.
|
| 15 |
MEYER-GESSNER M, BENKER G, LEDERBOGEN S, et al. Antithyroid drug-induced agranulocytosis: clinical experience with ten patients treated at one institution and review of the literature[J]. J Endocrinol Invest, 1994, 17(1): 29-36.
|
| 16 |
WIBERG J J, NUTTALL F Q. Methimazole toxicity from high doses[J]. Ann Intern Med, 1972, 77(3): 414-416.
|
| 17 |
KAMITANI F, NISHIOKA Y, KOIZUMI M, et al. Antithyroid drug-induced leukopenia and G-CSF administration: a long-term cohort study[J]. Sci Rep, 2023, 13(1): 19336.
|
| 18 |
NAKAMURA H, MIYAUCHI A, MIYAWAKI N, et al. Analysis of 754 cases of antithyroid drug-induced agranulocytosis over 30 years in Japan[J]. J Clin Endocrinol Metab, 2013, 98(12): 4776-4783.
|
| 19 |
COOPER D S. Agranulocytosis associated with antithyroid drugs[J]. Ann Intern Med, 1983, 98(1): 26.
|
| 20 |
AKAMIZU T, OZAKI S, HIRATANI H, et al. Drug-induced neutropenia associated with anti-neutrophil cytoplasmic antibodies (ANCA): possible involvement of complement in granulocyte cytotoxicity[J]. Clin Exp Immunol, 2002, 127(1): 92-98.
|
| 21 |
CHEN P L, SHIH S R, WANG P W, et al. Genetic determinants of antithyroid drug-induced agranulocytosis by human leukocyte antigen genotyping and genome-wide association study[J]. Nat Commun, 2015, 6: 7633.
|
| 22 |
CHEUNG C L, SING C W, TANG C S, et al. HLA-B*38: 02: 01 predicts carbimazole/methimazole-induced agranulocytosis[J]. Clin Pharmacol Ther, 2016, 99(5): 555-561.
|
| 23 |
ZHANG J J, YAN X J, LI Y, et al. Reactive plasmacytosis mimicking multiple myeloma associated with SFTS virus infection: a report of two cases and literature review[J]. BMC Infect Dis, 2018, 18(1): 528.
|
| 24 |
ABRAMSON H N. Immunotherapy of multiple myeloma: current status as prologue to the future[J]. Int J Mol Sci, 2023, 24(21): 15674.
|
| 25 |
ZHONG W H, ZHANG X Y, ZHAO M, et al. Advancements in nanotechnology for the diagnosis and treatment of multiple myeloma[J]. Biomater Sci, 2020, 8(17): 4692-4711.
|
| 26 |
李景岗. 多发性骨髓瘤与反应性浆细胞增多症临床表现及细胞形态学鉴别[J]. 吉林医学, 2012, 33(6): 1172-1173.
|
| 27 |
杨 红. 多发性骨髓瘤与反应性浆细胞增多症细胞形态学的探讨[J]. 中国实用医药, 2015, 10(20): 22-23.
|
| 28 |
郭慧霞, 王立茹, 邢嘉屿, 等. 达雷妥尤单抗治疗多发性骨髓瘤致乙肝病毒再激活1例报告并文献复习[J]. 中国实用内科杂志, 2024, 44(7): 614-616.
|
 ),Xin QI1,Sitong LIN2,Xiangwen SAN1,Ling JIN1,Sitong ZHANG1
),Xin QI1,Sitong LIN2,Xiangwen SAN1,Ling JIN1,Sitong ZHANG1