Journal of Jilin University(Medicine Edition) ›› 2023, Vol. 49 ›› Issue (3): 697-705.doi: 10.13481/j.1671-587X.20230319
• Research in basic medicine • Previous Articles Next Articles
Regulatory effect of lncRNA MALAT1 on activation of hepatic stellate cell and its mechanism
Lingyao XU,Shutang WEI,Yong DONG,Zhenglu SUN,Junbo ZHAO,Dazheng HAN( )
)
- Department of Gastroenterology,First Affiliated Hospital,Henan University,Kaifeng 475100,China
-
Received:2022-06-23Online:2023-05-28Published:2023-06-20 -
Contact:Dazheng HAN E-mail:13569519096@163.com
CLC Number:
- R575
Cite this article
Lingyao XU,Shutang WEI,Yong DONG,Zhenglu SUN,Junbo ZHAO,Dazheng HAN. Regulatory effect of lncRNA MALAT1 on activation of hepatic stellate cell and its mechanism[J].Journal of Jilin University(Medicine Edition), 2023, 49(3): 697-705.
share this article
Tab.1
General informations of subjects in various groups"
| Group | n | Age(year) | Gender[n(η/%)] | Hepatitis C virus[n(η/%)] | Serum alanine aminotransferase[λB/(U·L-1)] | Serum aspartate aminotransferase[λB/(U·L-1)] | ||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Yes | No | |||||
| Healthy | 25 | 54.39 | 12(48.0) | 13(52.0) | - | - | 35.47±17.10 | 37.58±18.23 |
| Mild fibrosis | 12 | 54.67 | 7(58.3) | 5(41.7) | 3(25.0) | 9(72.0) | 90.98±54.16 | 97.32±64.53 |
| Severe fibrosis | 13 | 55.58 | 6(46.2) | 7(53.8) | 4(30.8) | 9(69.2) | 134.25±86.29 | 148.65±74.82 |
| “-”:No data. | ||||||||
Tab.3
Expression levels of MALAT1, miR-150-5p and CXCL14 mRNA in HSC in various groups"
| Group | MALAT1 | miR-150-5p | CXCL14 mRNA |
|---|---|---|---|
| Control | 1.05±0.03 | 1.02±0.04 | 1.01±0.05 |
| TGF-β1 | 3.77±0.21* | 0.28±0.03* | 2.89±0.20* |
| TGF-β1+si-NC | 3.59±0.17 | 0.31±0.05 | 2.61±0.16 |
| TGF-β1+si-MALAT1 | 1.64±0.12△ | 0.75±0.06△ | 1.42±0.11△ |
| TGF-β1+si-MALAT1+anti-miR-150-5p | 1.56±0.13 | 0.46±0.04# | 1.89±0.12# |
| TGF-β1+si-MALAT1+CXCL14 | 1.78±0.15 | 0.68±0.04 | 2.05±0.15# |
Tab.4
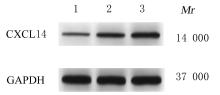
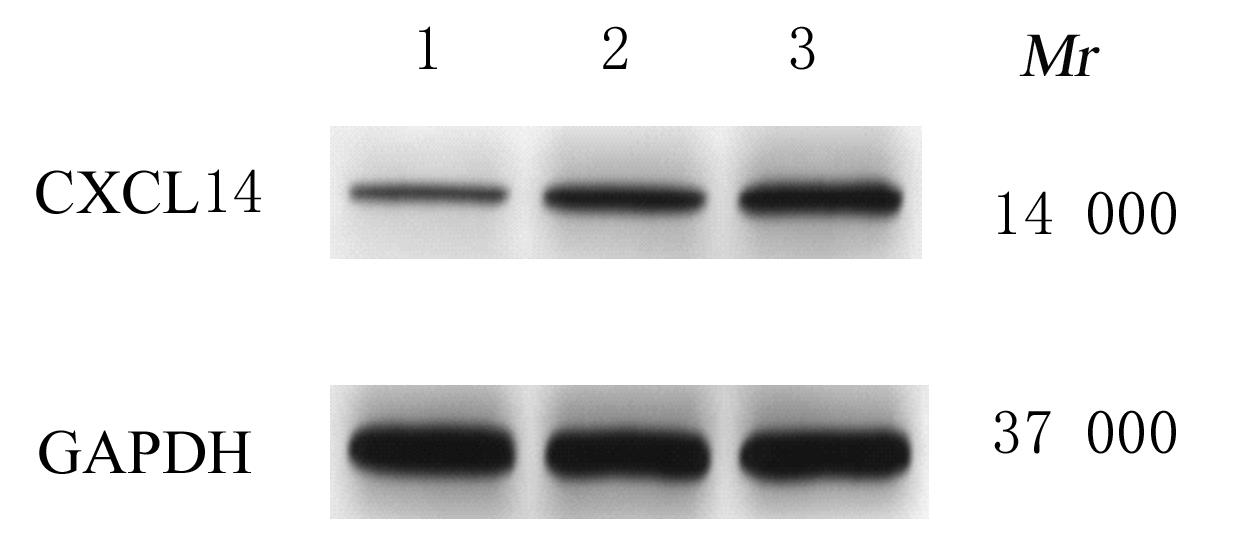
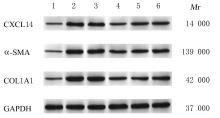
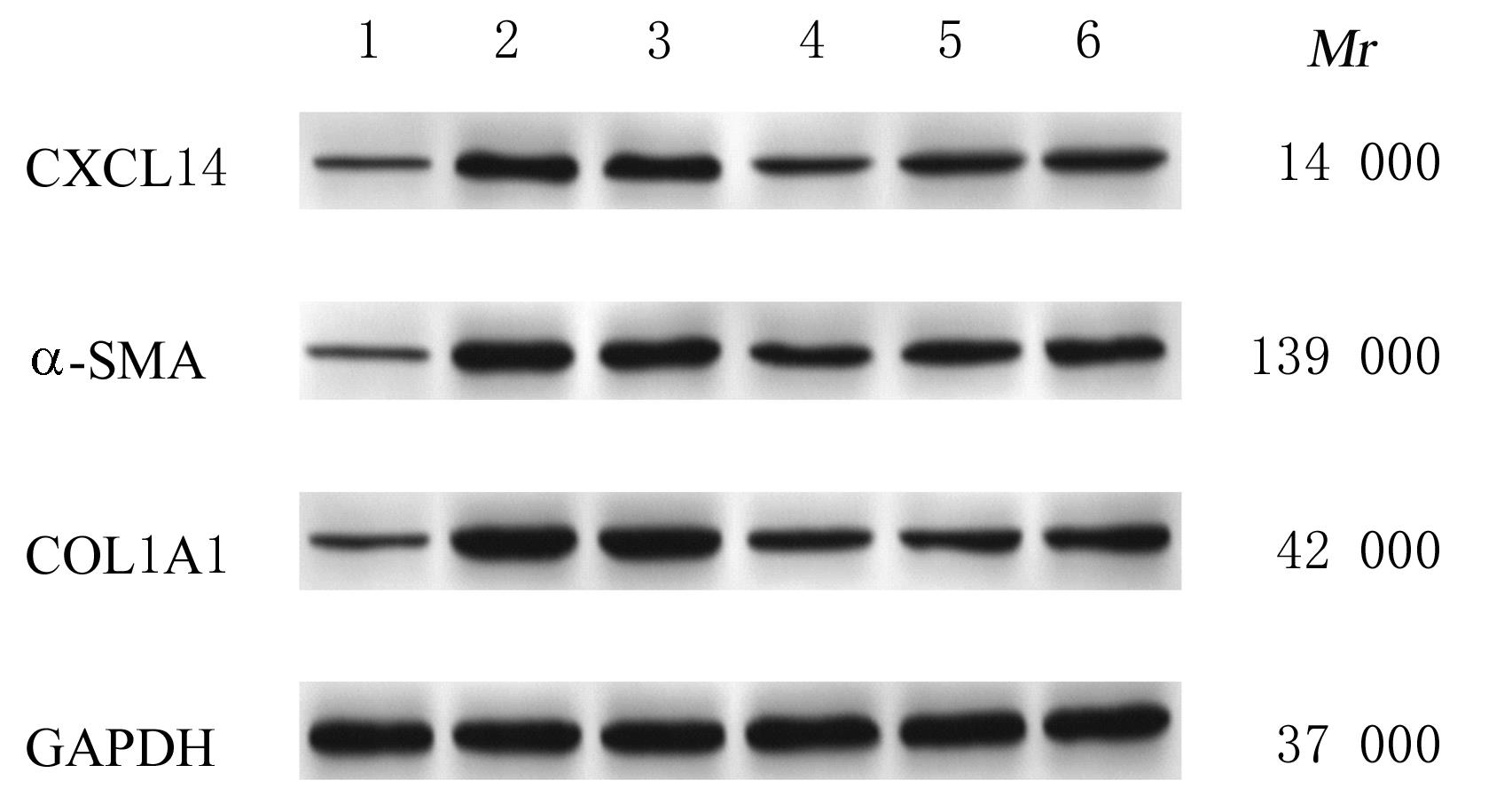
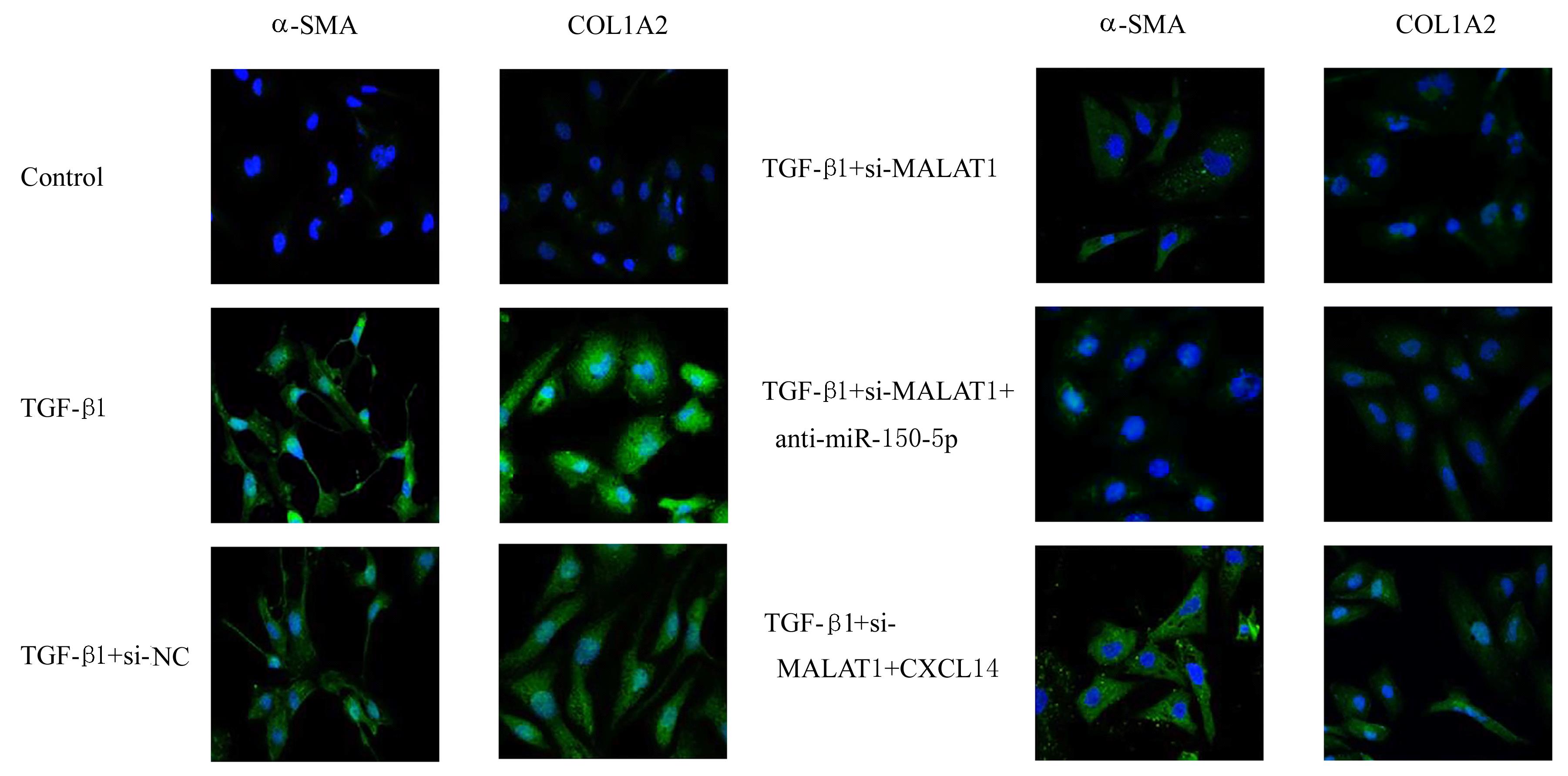
Expression levels of CXCL14, α-SMA, and COL1A1 proteins in HSC in various groups"
| Group | CXCL14 | α-SMA | COL1A1 |
|---|---|---|---|
| Control | 0.31±0.02 | 0.28±0.02 | 0.36±0.03 |
| TGF-β1 | 0.89±0.06* | 0.95±0.07* | 1.03±0.08* |
| TGF-β1+si-NC | 0.80±0.07 | 0.88±0.06 | 0.96±0.07 |
| TGF-β1+si-MALAT1 | 0.44±0.03△ | 0.50±0.03△ | 0.48±0.04△ |
| TGF-β1+si-MALAT1+anti-miR-150-5p | 0.59±0.04# | 0.65±0.05# | 0.66±0.06# |
| TGF-β1+si-MALAT1+CXCL14 | 0.65±0.05# | 0.71±0.06# | 0.76±0.05# |
| 1 | CASULLERAS M, ZHANG I W, LÓPEZ-VICARIO C,et al. Leukocytes, systemic inflammation and immunopathology in acute-on-chronic liver failure[J]. Cells, 2020, 9(12): 2632. |
| 2 | BOLDEANU M V, SILOŞI I, BĂRBULESCU A L, et al.Host immune response in chronic hepatitis C infection: involvement of cytokines and inflammasomes[J].Revue Roumaine De Morphol Embryol, 2020, 61(1): 33-43. |
| 3 | JIANG Y, XIANG C, ZHONG F, et al. Histone H3K27 methyltransferase EZH2 and demethylase JMJD3 regulate hepatic stellate cells activation and liver fibrosis[J]. Theranostics, 2021, 11(1): 361-378. |
| 4 | MORENO J A, HAMZA E, GUERRERO-HUE M, et al. Non-coding RNAs in kidney diseases: the long and short of them[J]. Int J Mol Sci, 2021, 22(11): 6077. |
| 5 | HAN S, ZHANG T, KUSUMANCHI P, et al. Long non-coding RNAs in liver diseases: focusing on nonalcoholic fatty liver disease, alcohol-related liver disease, and cholestatic liver disease[J]. Clin Mol Hepatol, 2020, 26(4): 705-714. |
| 6 | WU Y T, LIU X J, ZHOU Q, et al. Silent information regulator 1 (SIRT1) ameliorates liver fibrosis via promoting activated stellate cell apoptosis and reversion[J]. Toxicol Appl Pharmacol, 2015, 289(2): 163-176. |
| 7 | JIANG R, ZHOU Y J, WANG S F, et al. Nicotinamide riboside protects against liver fibrosis induced by CCl4 via regulating the acetylation of Smads signaling pathway[J]. Life Sci, 2019, 225: 20-28. |
| 8 | WANG Y H, MOU Q J, ZHU Z X, et al. MALAT1 promotes liver fibrosis by sponging miR‑181a and activating TLR4‑NF‑κB signaling[J]. Int J Mol Med, 2021, 48(6): 215. |
| 9 | DAI X Y, CHEN C, XUE J C, et al. Exosomal MALAT1 derived from hepatic cells is involved in the activation of hepatic stellate cells via miRNA-26b in fibrosis induced by arsenite[J]. Toxicol Lett, 2019, 316: 73-84. |
| 10 | OU M H, ZHAO H D, JI G X, et al. Long noncoding RNA MALAT1 contributes to pregnancy-induced hypertension development by enhancing oxidative stress and inflammation through the regulation of the miR-150-5p/ET-1 axis[J]. FASEB J, 2020, 34(5): 6070-6085. |
| 11 | LIAO J M, ZHANG Z, YUAN Q, et al. A lncRNA Gpr137b-ps/miR-200a-3p/CXCL14 axis modulates hepatic stellate cell (HSC) activation[J]. Toxicol Lett, 2021, 336: 21-31. |
| 12 | ZHAN W, LIAO X, CHEN Z S, et al. Leucine-rich repeats and immunoglobulin 1 (LRIG1) ameliorates liver fibrosis and hepatic stellate cell activation via inhibiting sphingosine kinase 1 (SphK1)/sphingosine-1-phosphate (S1P) pathway[J]. Iran J Allergy Asthma Immunol, 2020, 19(4): 397-408. |
| 13 | VALLET-PICHARD A, MALLET V, POL S. FIB-4: a simple, inexpensive and accurate marker of fibrosis in HCV-infected patients[J].Hepatology,2006,44(3): 769. |
| 14 | JI P, DIEDERICHS S, WANG W B, et al. MALAT-1, a novel noncoding RNA, and thymosin beta4 predict metastasis and survival in early-stage non-small cell lung cancer[J]. Oncogene, 2003, 22(39): 8031-8041. |
| 15 | WANG Z Q, WANG X J, ZHANG T Q, et al. LncRNA MALAT1 promotes gastric cancer progression via inhibiting autophagic flux and inducing fibroblast activation[J]. Cell Death Dis, 2021, 12(4): 368. |
| 16 | WANG N, CAO S J, WANG X X, et al. lncRNA MALAT1/miR‑26a/26b/ST8SIA4 axis mediates cell invasion and migration in breast cancer cell lines[J]. Oncol Rep, 2021, 46(2): 181. |
| 17 | TAN S, CHEN J L. Si-MALAT1 attenuates thymic cancer cell proliferation and promotes apoptosis via the miR-145-5p/HMGA2 pathway[J]. Oncol Lett, 2021, 22(2): 585. |
| 18 | LIU P H, ZHANG B, CHEN Z, et al. m6A-induced lncRNA MALAT1 aggravates renal fibrogenesis in obstructive nephropathy through the miR-145/FAK pathway[J]. Aging, 2020, 12(6): 5280-5299. |
| 19 | WANG H W, ZHENG X X, JIN J, et al. LncRNA MALAT1 silencing protects against cerebral ischemia-reperfusion injury through miR-145 to regulate AQP4[J]. J Biomed Sci, 2020, 27(1): 40. |
| 20 | ZHOU X J, ZHAO S, LI W, et al. Tubular cell-derived exosomal miR-150-5p contributes to renal fibrosis following unilateral ischemia-reperfusion injury by activating fibroblast in vitro and in vivo [J]. Int J Biol Sci, 2021, 17(14): 4021-4033. |
| 21 | CHE H, WANG Y Q, LI Y, et al. Inhibition of microRNA-150-5p alleviates cardiac inflammation and fibrosis via targeting Smad7 in high glucose-treated cardiac fibroblasts[J]. J Cell Physiol, 2020, 235(11): 7769-7779. |
| 22 | DU Z Y, WU T C, LIU L S, et al. Extracellular vesicles-derived miR-150-5p secreted by adipose-derived mesenchymal stem cells inhibits CXCL1 expression to attenuate hepatic fibrosis[J]. J Cell Mol Med, 2021, 25(2): 701-715. |
| 23 | WANG S, SHUAI C, GAO S S, et al. Chemokine CXCL14 acts as a potential genetic target for liver fibrosis[J]. Int Immunopharmacol, 2020, 89(Pt A): 107067. |
| [1] | Mingliu GU,Fengyuan LIN,Xuefeng WU,Jianing ZHOU,Xuechun LU,Peige DU,Liping AN. Improvement effect of Phellinus igniarius acidic polysaccharide on liver fibrosis induced by bile duct ligation in mice and its mechanism [J]. Journal of Jilin University(Medicine Edition), 2022, 48(5): 1167-1174. |
| [2] | Zhouguang WU,Bin WANG,Zhen CHENG,Wenjie ZHANG,Taoyan ZUO,Siqi CHEN,Jingru FU. Analysis on correlation of GPC3 and α-SMA expressions with liver function-related indexes in liver tissue of children with biliary atresia [J]. Journal of Jilin University(Medicine Edition), 2021, 47(5): 1237-1243. |
| [3] | Yang ZHENG,Jiahui WANG,Yue PENG,Xianling YUAN,Lei WANG,Tiejian ZHAO. Influence of curcumol in structure of liver sinusoidal endothelial cells of mice and its inhibitiory effect on intrahepatic angiogenesis [J]. Journal of Jilin University(Medicine Edition), 2021, 47(5): 1124-1130. |
| [4] | Rongjun JIA,Liman MA,Lihua LI. Protective effect of calcitriol on hepatic fibrosis induced by bile duct ligation in mice and its mechanism [J]. Journal of Jilin University(Medicine Edition), 2021, 47(2): 257-264. |
| [5] | YANG Fan, LI Lihua. Effect of vitamin D receptor activation on hepatic fibrosis induced by bile duct ligation in mice and its mechanism [J]. Journal of Jilin University(Medicine Edition), 2020, 46(04): 722-727. |
| [6] | XIE Jing, LI Lihua. Inhibitory effect of dehydroandrographolide on hepatocyte apoptosis induced by carbon tetrachloride in hepatic fibrosis model mice and its mechanism [J]. Journal of Jilin University(Medicine Edition), 2019, 45(05): 1009-1014. |
| [7] | BAI Jie, JI Wenjing, DING Yongnian, PENG Yuanyuan, CHEN Yuanwen. Changes of levelsof endogenous AcSDKP and its regulatory factors in liver tissue of model rats with liver fibrosis induced by bile duct ligation [J]. Journal of Jilin University(Medicine Edition), 2018, 44(05): 999-1004. |
| [8] | CHANG Caifang, HOU Yong, CONG Gang. Therapeutic effect of α-2b interferon on inflammation of liver tissue and liver fibrosis in hepatitis B model ducks [J]. Journal of Jilin University Medicine Edition, 2017, 43(01): 11-15. |
| [9] | YANG Kun, TIAN Zhenzhen, WANG Shuhua, XIU Ming, GUO Xiangling, QI Lina, LI Min, SUN Li, GAO Runping. Effect of LPS-TLR4 pathway in hepatic fibrogenesis of rats with chronic alcohol intake [J]. Journal of Jilin University Medicine Edition, 2015, 41(04): 751-755. |
| [10] | HAO Xiaofang, ZHANG Ronghua, WANG Lin, WANG Meimei, ZHEN Yongzhan, ZHANG Guangling, CHEN Jing. Therapeutic effect of rhein lysinate on liver fibrosis in cholestatic model rats and its molecular mechanisms [J]. Journal of Jilin University Medicine Edition, 2015, 41(03): 481-485. |
| [11] | ZHONG Zhi-hong,YAN Wen-zhen,DAI Dong,CHEN Tu-ming,HU Zu-chao. Therapeutic effect of rapamycin on liver fibrosis model rats induced by carbon tetrachloride oil [J]. Journal of Jilin University Medicine Edition, 2013, 39(6): 1224-1227. |
| [12] | DAI Yong-Mei, CAI Li-Mian, LIN Ling. Inhibitory effect of octreotide on prolieration of rat hepatic stellate cells [J]. J4, 2009, 35(6): 1052-1056. |
| [13] | QI Xiao-yan,GAO Run-ping,ZHANG Rui-juan,LI Guo-feng,YANG Yong-guang. Effects of hammerhad ribozyme targeting connective tissue growth factor on collagen Ⅰ synthesis and cell cycle progression of human hepatic stellate cells [J]. J4, 2009, 35(1): 26-29. |
| [14] | ZHANG Yi-ning, NIU Jun-qi, DING Yan-hua, WANG Feng. Anti-oxidative stress effects of Taurine on rat hepatic stellate cells [J]. J4, 2005, 31(2): 179-181. |