吉林大学学报(医学版) ›› 2025, Vol. 51 ›› Issue (2): 493-500.doi: 10.13481/j.1671-587X.20250224
• 临床医学 • 上一篇
骨性Ⅱ类错颌畸形伴OSAHS患者双颌前移术后上气道变化1例报告及文献复习
- 1.吉林大学口腔医院口腔整形美容外科,吉林 长春 130021
2.吉林大学口腔医院正畸科,吉林 长春 130021
Changes of upper airway in patient with skeletal class Ⅱ malocclusion accompanied by OSAHS after maxillomandibular advancement surgery: A case report and literature review
Xiangjin HU1,Xiumei SUN2,Kai CHEN1,Guomin WU1( )
)
- 1.Department of Oral,Plastic and Aesthetic Surgery,Stomatology Hospital,Jilin University,Changchun 130021,China
2.Department of Orthodontics,Stomatology Hospital,Jilin University,Changchun 130021,China
摘要:
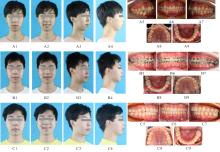
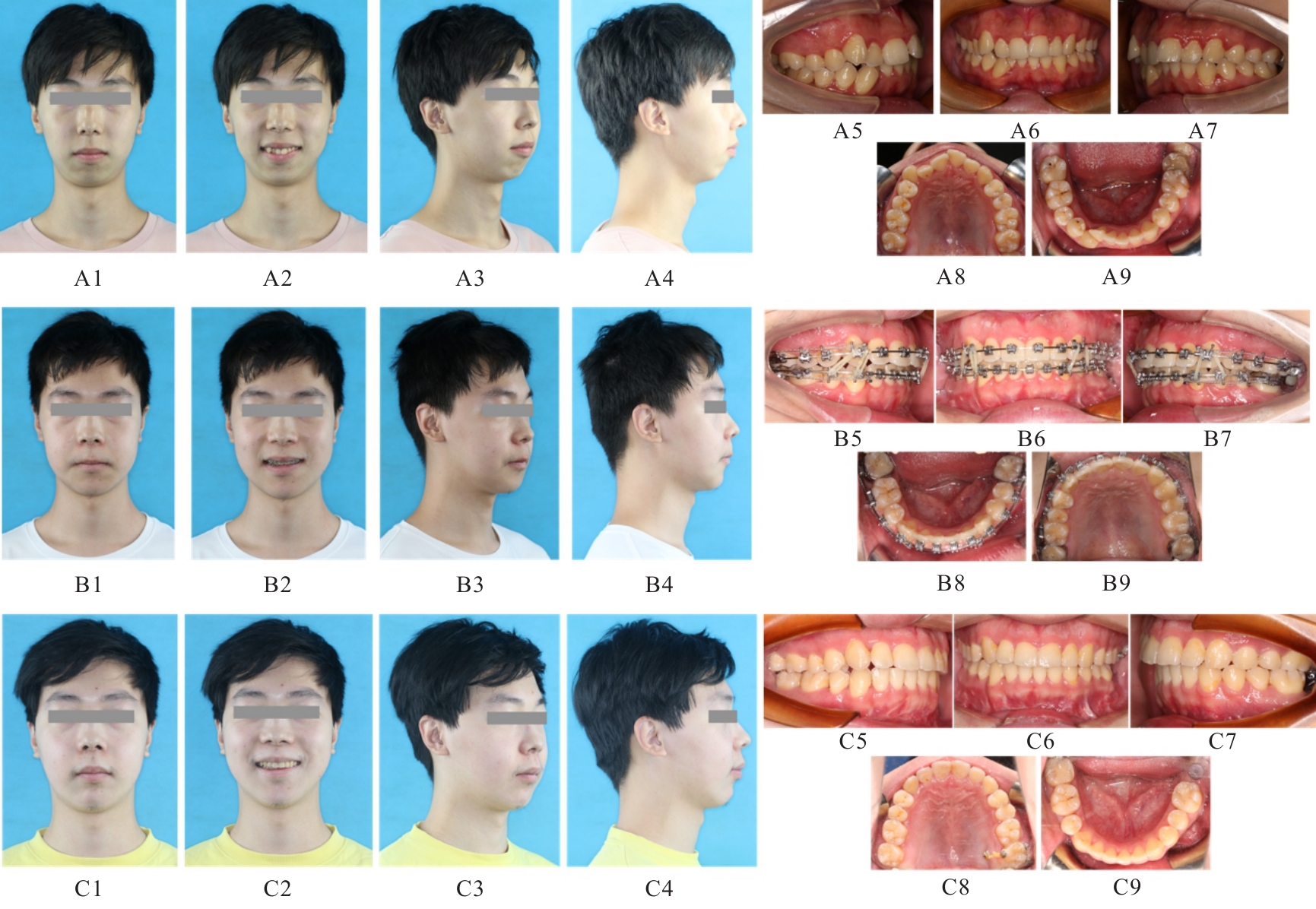
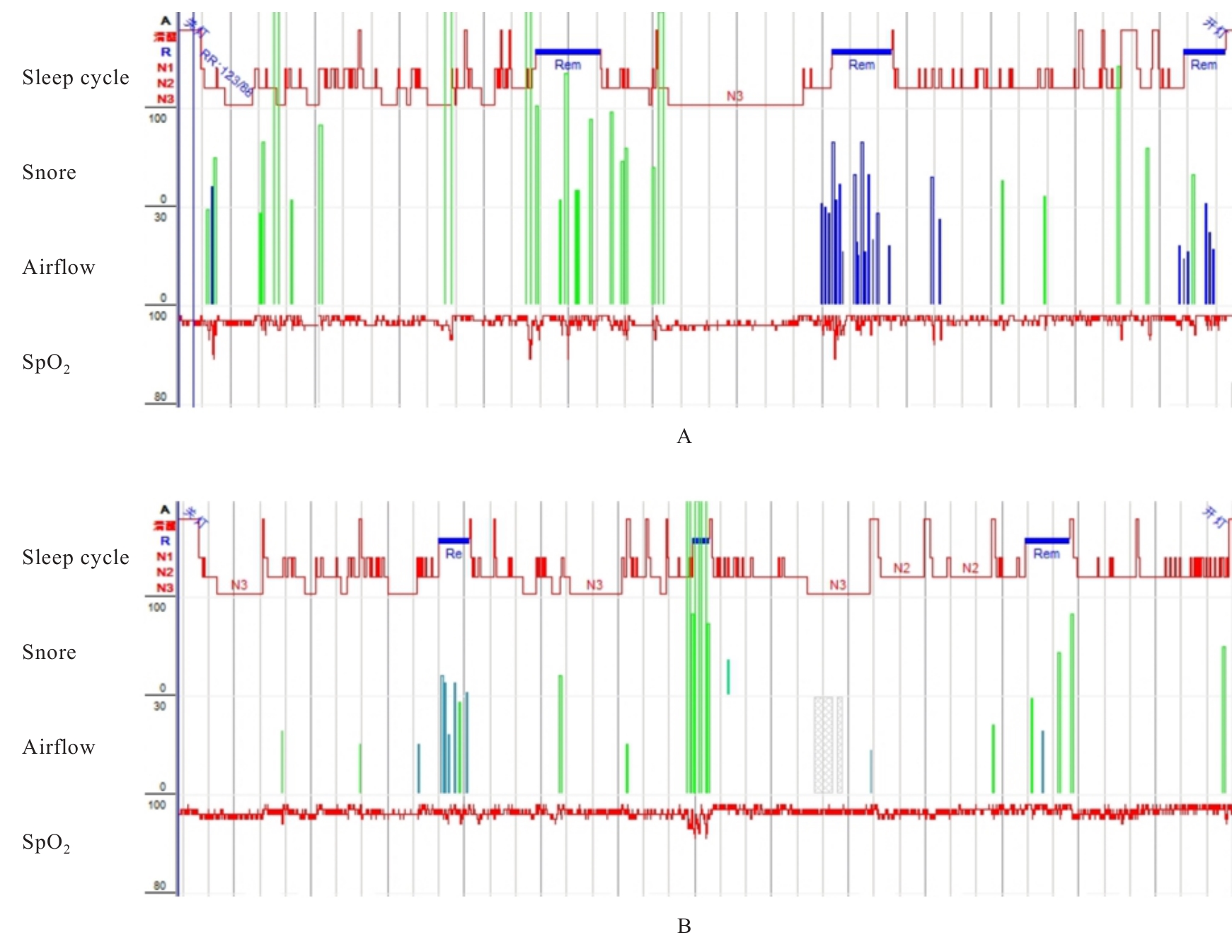
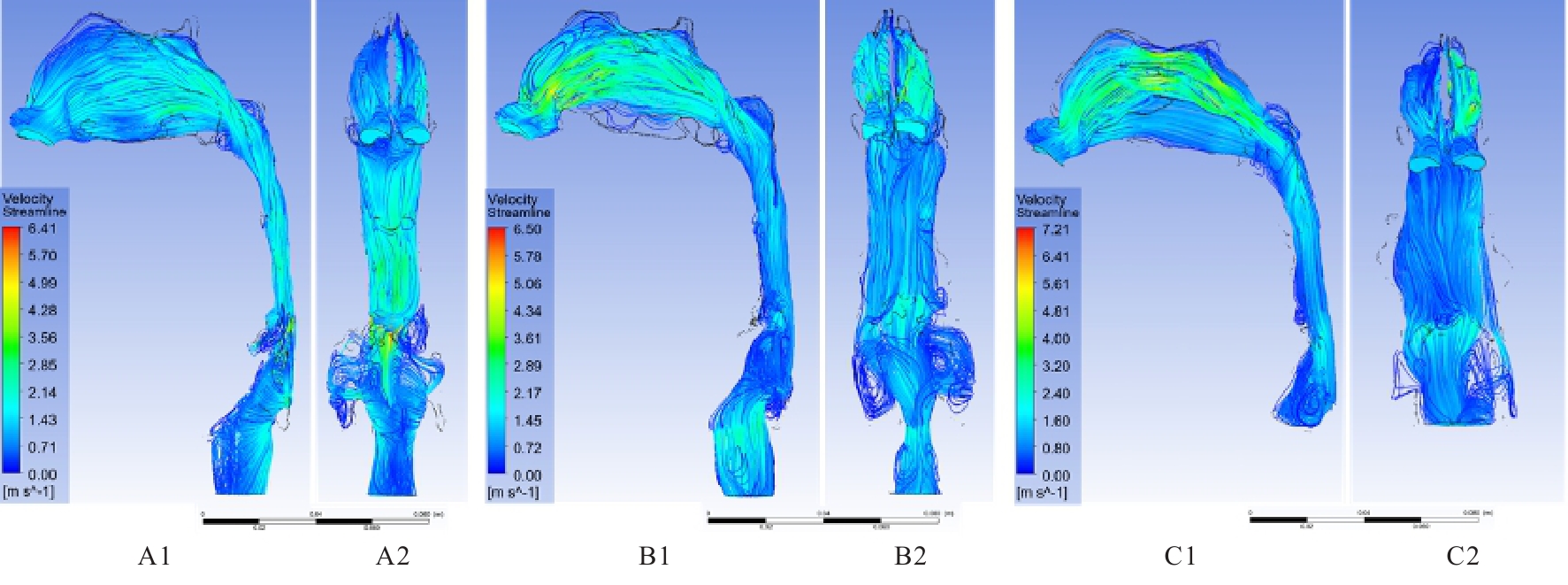
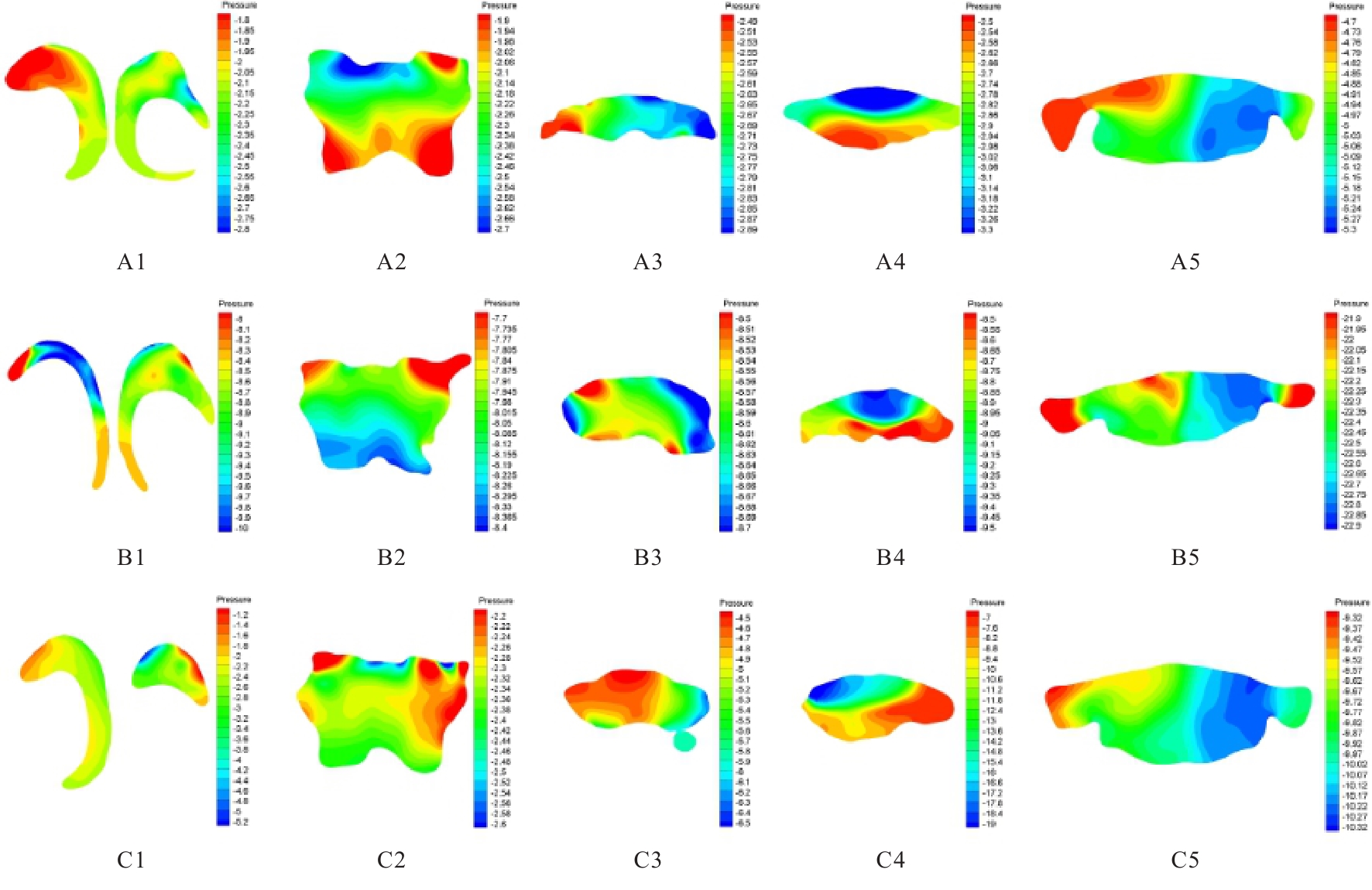
骨性Ⅱ类错颌畸形患者常伴有上气道的结构和功能异常,严重者可发生阻塞性睡眠呼吸暂停低通气综合征(OSAHS),本文作者观察1例骨性Ⅱ类错颌畸形伴OSAHS患者双颌前移(MMA)术后上气道发生的形态学和流体力学改变。患者,男性,27岁,骨性Ⅱ类错颌畸形伴中度OSAHS,采用正畸正颌联合治疗方案,前移上下颌骨,对比患者手术前后面相和口内相,可见咬合关系良好,覆颌覆盖和尖磨牙关系正常。上气道流场改善明显,术后2年鼻咽气道横截面积增加10.76%,压强降低55.36%;腭咽气道横截面积增加108.25%,压强降低98.14%;舌咽气道横截面积增加97.51%,压强降低351.03%;喉咽气道横截面积增加27.54%,压强降低95.62%。呼吸暂停和低通气指数(AHI)降低55.45%,基本达到治疗目标。形态学测量结合流体力学分析能够更加全面地评价上气道状况,计算流体力学(CFD)分析得到的上气道临界闭合压(Pcrit)近似值可作为评估上气道状况的一项简便的定量指标。
中图分类号:
- R782.2