吉林大学学报(医学版) ›› 2025, Vol. 51 ›› Issue (6): 1670-1678.doi: 10.13481/j.1671-587X.20250623
• 临床研究 • 上一篇
乳腺癌相关参数联合腋窝淋巴结超声阳性特征对淋巴结转移负荷的预测价值
常乾坤1,吴文瑛1( ),白春强1,丁智超2,王伟芳3,刘铭函4
),白春强1,丁智超2,王伟芳3,刘铭函4
- 1.承德医学院附属医院南院区超声科,河北 承德 067020
2.河北省承德市中心医院放射科,河北 承德 067024
3.河北省承德市中心医院超声科,河北 承德 067024
4.河北省承德市中医院功能科,河北 承德 067032
Predictive value of breast cancer related parameters combined with positive axillary lymphnode ultrasound features for lymphnode metastasis burden
Qiankun CHANG1,Wenying WU1( ),Chunqiang BAI1,Zhichao DING2,Weifang WANG3,Minghan LIU4
),Chunqiang BAI1,Zhichao DING2,Weifang WANG3,Minghan LIU4
- 1.Department of Ultrasonic Diagnosis,Affiliated Hospital,Chengde Medical University,Chengde 067020,China
2.Department of Radiology,Central Hospital,Chengde City,Hebei Province,Chengde 067024,China
3.Department of Ultrasonic Diagnosis,Central Hospital,Chengde City,Hebei Province,Chengde 067024,China
4.Functional Department,Traditional Chinese Medicine Hospital,Chengde City,Hebei Province,Chengde 067032,China
摘要:
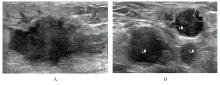
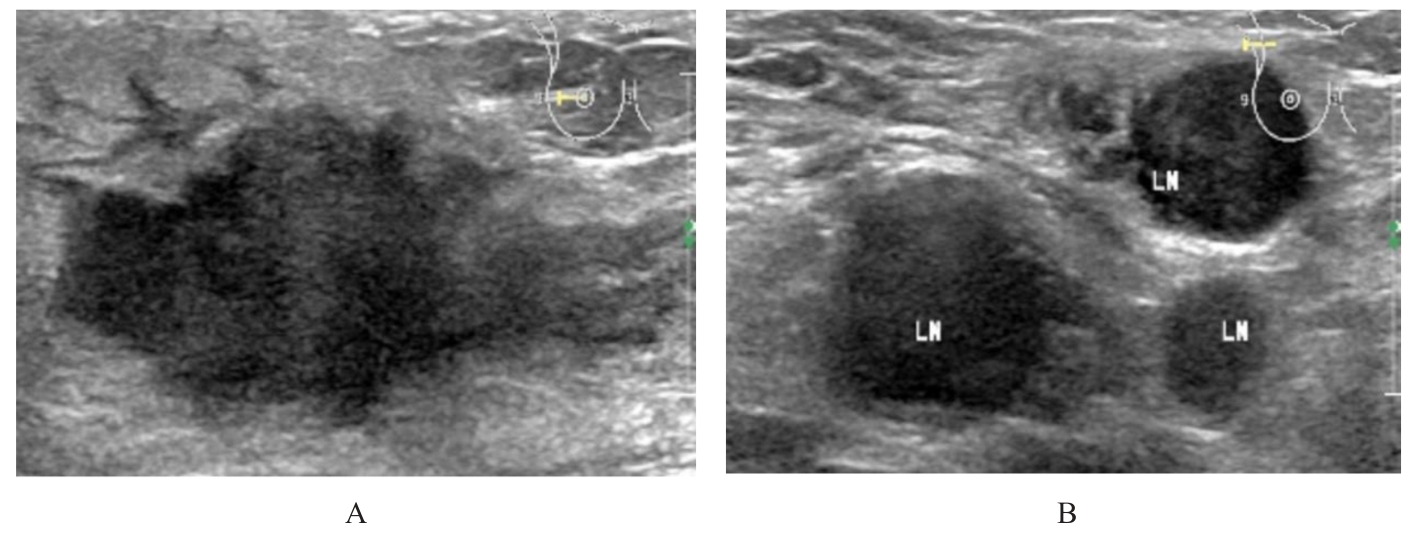
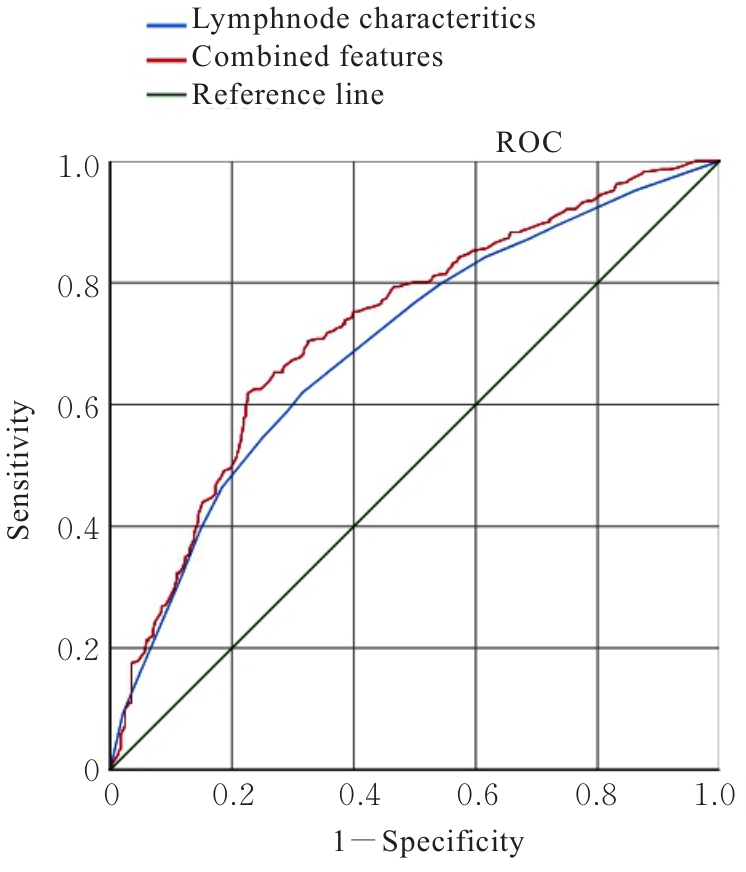
目的 分析乳腺癌相关参数及腋窝淋巴结阳性超声特征,探讨腋窝淋巴结转移负荷的危险因素,为乳腺癌患者术前评估提供依据。 方法 回顾性分析经手术病理证实存在腋窝淋巴结转移的574例乳腺癌患者的超声和临床病理资料,根据腋窝淋巴结转移情况,分为低淋巴结负荷(LNB)组(n=283)和高淋巴结负荷(HNB)组(n=291)。比较2组患者患侧、肿物所在象限、距皮肤距离、最大径线、内部回声、形态、边缘、钙化、血供、后方回声、淋巴结长径、淋巴结短径、淋巴结纵横比、可疑转移数量、淋巴结内血供、淋巴结门形态、年龄、病理类型、组织学分级、分子分型及雌激素受体(ER)、孕激素受体(PR)、Ki-67、人表皮生长因子受体2(HER2)和P53表达情况。采用Logistic回归分析乳腺癌患者腋窝淋巴结转移负荷的危险因素,采用受试者工作特征(ROC)曲线和曲线下面积(AUC)评价预测价值。 结果 单因素分析,2组患者肿物所在象限、距皮肤距离、分子分型、HER2阳性表达、淋巴结长径、淋巴结短径、淋巴结纵横比、可疑转移数量和淋巴结门形态比较差异有统计学意义(P<0.05)。多因素Logistic回归分析,肿物位于外上象限(OR=0.648,P=0.021)、距皮肤距离<5 mm(OR=0.283,P=0.016)、Luminal A(OR=1.564,P=0.044)、淋巴结长径≥20 mm(OR=2.050,P<0.01)、淋巴结短径≥8.6 mm(OR=2.430,P<0.01)、淋巴结纵横比<2(OR=1.585,P<0.01)和淋巴结门形态不清晰(OR=2.092,P<0.01)是腋窝淋巴结转移负荷的独立危险因素。ROC曲线分析,与腋窝淋巴结阳性超声特征比较,乳腺癌相关参数联合腋窝淋巴结阳性超声特征的AUC较大(Z=2.72,P=0.006 5),对腋窝淋巴结转移负荷的预测价值更高。 结论 乳腺癌所在象限、距皮肤距离、分子分型、淋巴结长径、淋巴结短径、淋巴结纵横比和淋巴结门形态是腋窝淋巴结转移负荷的独立危险因素,对腋窝淋巴结转移负荷有一定预测价值。
中图分类号:
- R445.1